OTHER CELLULITE TREATMENTS
Content extracted from the book “Victory Against Cellulite” by Dr Roberto Chacur, Ed. AGE, 2023.
Dr. Cibele Tamietti Durães
Dr. Roberto Chacur
Cellulite is a multifactorial condition caused by hormonal aspects, circulation difficulties, fat accumulation, sagging and fibrosis formation. An effective intervention therefore depends on the treatment of each of these causes, according to the needs of each patient. Several treatments can and should be combined to treat cellulite. They can be classified as non-invasive, minimally invasive and surgical, and can be associated with each other in a specific treatment protocol for each patient, with the objective of improving skin health as a whole. In addition to the methods that will be described in this chapter, it is important to associate them with the adoption of healthy habits, such as regular physical activity and a balanced diet. According to the Body Mass Index (BMI), follow-up with a nutritionist, nutrologists or endocrinologists may be necessary to correct the index and thus obtain better results.
See Chapters
CHAPTER 1 - DEFINITION, HISTORY AND NOMENCLATURE
CHAPTER 2 - ONLINE QUESTIONNAIRE FOR CELLULITE CLASSIFICATION
CHAPTER 3 - LIPEDEMA: DESCRIPTION, DIAGNOSIS AND TREATMENT
CHAPTER 4 - ANATOMY OF THE GLUTE REGION APPLIED IN PRACTICE
CHAPTER 6 - INJECTABLE CELLULITE TREATMENTS
CHAPTER 7 - LASER-LIPO: INVASIVE TECHNOLOGY
CHAPTER 8 - OTHER CELLULITE TREATMENTS
CHAPTER 9 - BIOSTIMULATORY EFFECTS OF MICROSPHERE INJECTIONS INTO OVERLYING SKIN STRUCTURES
CHAPTER 10 - INFLUENCE OF HORMONES ON CELLULITE: WITH EMPHASIS ON ADIPONECTIN
CHAPTER 11 - GOLDINCISION®: A MULTIFACTORIAL APPROACH TO THE TREATMENT OF CELLULITE
CHAPTER 12 - STAINS POST-GOLDINCISION®
CHAPTER 13 - ADVERSE EFFECTS AND COMPLICATIONS IN GOLDINCISION®
With the collaboration of experienced medical professionals, Dr. Roberto Chacur brings together in this book an approach around the theme ranging from the genesis of cellulite, the proper method of evaluating and classifying, associated diseases and hormonal modulation to existing treatments, what really works and why the GOLDINCISION method is considered the gold standard.
NON-INVASIVE TREATMENTS
Topical treatments
Topical therapies serve as adjuvants in the treatment of cellulite. They are not effective alone, since they only have a transitory effect, without acting on the retraction caused by the fibrous septa. There are numerous cosmeceutical and herbal ingredients that act on adipocytes, favoring lipolysis, in the interstitium, or in the microcirculation of cellulite. Those that act on adipocytes are beta-agonists (represented by methylxanthines), which, by inhibiting the activity of the phosphodiesterase enzyme, have the potential to induce lipolysis, alpha-adrenergic inhibitors (yohimbine, piperoxana, phentolamine, di- hydroergotamine) and adenylcyclase activators (thyroid hormones, some algae and organic silicon).
Among those that act in the interstices, we can mention organic silicon, Centella asiatica, ascorbic acid, some enzymes and algae, tretinoin and retinol. Retinoids inhibit metalloproteinases, which damage collagen structure and stimulate elastin production, increasing collagen thickness, improving elastic fibers and inhibiting the differentiation of adipocyte precursor cells. The substances that act on the microcirculation are herbal medicines, such as flavonoids, saponins, coumarins and pentoxifyllines. These botanical extracts improve local microcirculation and reduce blood viscosity, platelet growth factor; thus decreasing capillary permeability and improving vessel wall tonus.
The supporting effects of the topics used include the stimulation of the peripheral microcirculation, the promotion of lipolysis, the increase in dermal neocollagenesis, the lymphatic drainage and the reduction of edema.
Oral treatments
Oral therapies are often questioned about their effectiveness, however, just as in the case of topical treatments, they act as adjuvants in the treatment of cellulite. This type of treatment mainly plays the role of nutritional supplements, which can act as an antioxidant; cell metabolism stimulator and body weight control, such as lipophilic, collagen and elastin synthesis stimulators; and as a reducer of edema and inflammation.
In view of this, here are some examples in the literature of substances indicated in the management of GLD.
REFERENCES
Altmeyer MD, Anderson LL, Wang AR. Silicone migration and granuloma formation. J Cosmet Dermatol. 2009;8:92– 97. [PubMed] [Google Scholar] Badin AZ, Vieira JF. Endoscopically assisted buttocks augmentation. Aesthetic Plast Surg. 2007;31:651–656. [PubMed] [Google Scholar]
Blanco Souza T, Colomé L, Bender EA, Lemperle G. Brazilian consensus recommendation on the use of polymeth- ylmetacrylate filler in facial and corporal aesthetics.
Aesth Plast Surg. 2018;42:1244–1251 [PubMed] [Google Scholar]
Cárdenas-Camarena L, Arenas-Quintana R, Robles-Cervantes JA. Buttocks fat grafting: 14 years of evolution and experience. Reconstr Surg. 2011;128:545–555. [PubMed][Google Scholar]
Chacur R. Ciência e Arte do Preenchimento. 2018, 1.ed Porto Alegre: AGE; 262. [Google Scholar] Chong T, Coon D, Toy J, et al. Body contouring in the male weight loss population: assessing gender as a factor in outcomes. Plast Reconstr Surg. 2012;130:325e–330e.
[PubMed] [Google Scholar] Cruse PJ, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206–210. [PubMed] [Google Scholar]
Duscher D, Kiesl D, Aitzetmüller MM, et al. Seasonal impact on surgical-site infections in body contouring surgery: a retrospective cohort study of 602 patients over a period of 6 years. Plast Reconstr Surg. 2018;142:653–660.[PubMed] [Google Scholar]
Frazer RQ, Byron RT, Osborne PB et al. PMMA: an essential material in medicine and dentistry. J Long Term Eff Med Implants. 2005;15:629–639. [PubMed] [Google Scholar]
Gonzales R. Intramuscular gluteal augmentation: the XYZ method. Clin Plastic Surg. 2018;45:217–223. [PubMed] [Google Scholar]
González-Ulloa M. Gluteoplasty: a ten-year report. Aes- thetic Plast Surg. 1991;15:85–91. [PubMed] [Google Scholar] Gruskay J, Smith J, Kepler CK et al. The seasonality of post- operative infection in spine surgery. J Neurosurg Spine.
2013;18:57–62. [PubMed] [Google Scholar] Harrison D, Selvaggi G. Gluteal augmentation surgery: indications and surgical management. J Plast Reconstr Aesthet Surg. 2007;60:922–928. [PubMed] [Google Scholar] Hilinski JM, Cohen SR. Soft tissue augmentation with Arte-
Fill. Facial Plast Surg. 2009;25:114–119. [PubMed] [Google Scholar] Jaimovich CA, Almeida MW, Aguiar LF et al. Internal suture technique for improving projection and stability in sec- ondary gluteoplasty. Aesthet Surg J. 2010;30:411–413.
[PubMed] [Google Scholar] Lee YB, Park SM, Song EJ, et al. Histology of a novel injectable filler (polymethylmethacrylate and cross-linked dextran in hydroxypropyl methylcellulose) in a rat model.J Cosmet Laser Ther. 2014;16:191–196. [PubMed] [Google Scholar]
Lemperle G, Morhenn V, Charrier U. Human histology and persistence of various injectable filler substances for softtissue augmentation. Aesthetic Plast Surg. 2003;27:354– 366; discussion 367. [PubMed] [Google Scholar]
McClelland M, Egbert B, Hanko V et al. Evaluation of artecoll polymethylmethacrylate implant for soft-tissue aug- mentation: biocompatibility and chemical characterization. Plast Reconstr Surg. 1997;100:1466–1474. [PubMed][Google Scholar] Mendieta CG. Gluteoplasty. Aesthet Surg J. 2003;23:441–455. [PubMed] [Google Scholar]
Oranges CM, Tremp M, di Summa PG, et al. Gluteal augmentation techniques: a comprehensive literature review. Aesthet Surg J. 2017;37:560–569. [PubMed] [Google Scholar]
Serra F, Aboudib JH, Cedrola JP, et al. Gluteoplasty: anatom- ic basis and technique. Aesthet Surg J. 2010;30:579–592.
[PubMed] [Google Scholar] Serra F, Aboudib JH, Marques RG. Intramuscular technique for gluteal augmentation: determination and quantification of muscle atrophy and implant position by computed tomographic scan. Plast Reconstr Surg. 2013;131:253e–259e. [PubMed] [Google Scholar]
Serra F, Aboudib JH, Marques RG. Reducing wound complications in gluteal augmentation surgery. Plast ReconstrSurg. 2012;130:706e–713e. [PubMed] [Google Scholar] Sozer SO, Agullo FJ, Palladino H. Autologous augmentation gluteoplasty with a dermal fat flap. Aesthet Surg J.
2008;28:70–76. [PubMed] [Google ScholarSozer SO, Agullo FJ, Palladino H. Split gluteal muscle flap for autoprosthesis buttock augmentation. Plast Reconstr Surg. 2012;129:766–776. [PubMed] [Google Scholar] Vergara R, Amezcua H. Intramuscular gluteal implants:
15 years’ experience. Aesthet Surg J. 2003;23:86–91. [PubMed] [Google Scholar]
PPAR agonists
Peroxisome proliferator-activated receptors (PPARs) are a family of nuclear transcription factors found in human keratinocytes and adipocytes that are activated by hypolipidemic drugs of fibrate, fatty acids, eicosanoids, and prostanoids. PPARs were identified for the first time in the epidermis in 1992 and their importance in epidermal homeostasis was subsequently discovered, showing that they can accelerate the formation of the epidermal barrier, induce epidermal differentiation and influence the biosynthesis of lipids, such as, for example, ceramides, in the skin. Scientific articles from 2006 highlight the benefits of a PPAR agonist, in particular petroselinic acid and conjugated linoleic acid (CLA®, Unilever patent), which act on epidermal differentiation, reducing inflammation, increasing extracellular matrix components and promoting improvements in signs of photodamage and skin tone. Although few studies have been conducted on cellulite, CLA® has been shown to reduce body fat mass in obese individuals, with a corresponding increase in lean body mass and improvement in the signs of cellulite.
Centella asiatica
Centella asiatica is a medicinal herb that is widely used in the East and is becoming popular in the West. In India, it is known as mandukparni or Indian pennywort, or jalbrahmi. In China, it is called gotu kola. The active constituents of Centella asiatica are saponins (also called triterpenoids); brahmoside and brahminoside; isothankuniside and thankuniside glycosides; plant sterols; flavonoids and other components without known pharmacological activity, such as abundant tannins (20-25%); essential acid (0.1% with beta-caryophyllene, trans-beta-farnesen and germacrene D); phytosterols (campesterol, sitosterol, stigmasterol); mucilages; resins; free amino acids (alanine, serine, aminobutyrate, aspartate, glutamate, lysine and threonine); flavonoids (derived from quercetin and kempferol); an alkaloid (hydrocotin); a bitter component (vallerin); and fatty acids (linoleic, linolelic, oleic, palmitic and stearic acids).

Ursane and oleanane-type triterpene oligoglycosides, such as centellasaponins B, C, and D, are also present in the plant, and although the mechanisms are not fully understood, it is highly likely that these agents are PPAR agonists. Several studies on Centella asiatica show its action in the human organism as antioxidants; adipocyte diameter reducers, mainly in the gluteal-femoral region and interadipocyte fibrosis; as a bactericide; anti-inflammatory; stimulant of collagen production; blood circulation activator; diuretic effect with improved fluid retention, among others. Therefore, it is indicated as an adjunct in the treatments of GLD.
Hydroxycitrate
Garcinia cambogia hydroxycitrate, also known as Malabar tamarind, is an inhibitor of lipogenesis and has been used alone or in conjunction with chromium linked to niacin or Gymnema sylvestre (ginemic acid) to help control and reduce body weight. Also, because it is a hydroxy acid, it helps with collagen synthesis. Due to these actions, its use is likely to improve the appearance of the GLD.
Green tea and polyphenols
Green tea comes from the leaves of the Camellia sinensis plant and contains a variety of phytochemicals. In general, 30% of the dry weight of leaves is composed of polyphenolic components, including flavonols, flavonoids and phenolic acids. Most polyphenols present in green tea are flavonols and, among these, catechins are predominant. The main catechins in green tea are: epigallocatechin-3-gallate (EGCG); epigallocatechin (EGC); epicatechin-3-gallate (ECG); and epicatechin (EC). Catechins (C), gallocatechins (GC), catechin gallate (CG) and gallocatechin gallate (GCG) can be epimerized during heat treatment.
Among green tea catechins, EGCG is the most abundant, constituting about one third of its total dry weight, and important properties against cancer, obesity, diabetes and inflammation are attributed to them. Green tea is considered the greatest bioactive component for weight reduction, with the effect of decreasing the differentiation and proliferation of adipocytes during lipogenesis. The mechanism by which green tea can reduce the percentage of body fat is still not fully elucidated, but there are several hypotheses, which include: increased expression of genes involved in the metabolism of fatty acids; inhibition of catechol-o-methyltransferase enzyme activity; increased oxidation of fats; improvement of thermogenesis markers; increased energy expenditure; stimulation of lipolysis; regulation of activities of endogenous antioxidant enzymes; decreased production of ROS (reactive oxygen species) and levels of inflammation in adipose tissue. However, there is no consensus on the ideal dose, duration of treatment and mode of administration for this type of tea-supplement, as studies vary greatly in these areas.

Camellia sinensis. (Source: NatashaG/pixabay.com (2022).
Although the effects of this tea on GLD have not been tested, as it is a topic of interest for the treatment of obesity, it has also been used as an adjuvant in GLD treatments.
Ginkgo biloba
Ginkgo biloba extract is a substance obtained from the leaves of the Ginkgo tree, native to Korea, China and Japan. This herbal medicine is rich in flavonoids and terpenoids; exerts strong anti-inflammatory and antioxidant action; and acts to improve arterial, cerebral and peripheral blood flow. Ginkgo biloba is used in the treatment of GLD because it has many effects on the peripheral circulation. This extract decreases blood viscosity, inhibits platelet activation factor, decreases vascular permeability and increases the deformability of red blood cells, improving microcirculation. It also acts against free radicals, activates cell metabolism and inhibits phosphodiesterase. Flavonoids act as antioxidants and anti-inflammatories, in addition to acting as arterial vasodilators and venous vasoconstrictors.Terpenes inhibit platelet activator, decrease vessel permeability and improve vascular wall tone.
Dimpless®
Dimpless® is derived from the French variety of cantaloupe melon, rich in superoxide dismutase (SOD) (representing about 85 to 90% of the total composition) and other primary antioxidants such as catalase (CAT) and glutathione peroxidase (GPx), and secondary ones, such as coenzyme Q10, lipoic acid, carotenoids, vitamins A, E and C.

Due to its superoxide dismutase (SOD) anti-fibrosis properties, Dimpless® is designed to reduce both the fibrous state and the size of adipocytes by stimulating lipolysis. In addition, Dimpless®, due to its components, has an anti-inflammatory action, acts on lipogenesis, favors the reconstruction of the extracellular matrix, reduces the size of adipocytes and reduces nodules and the accumulation of fat, thus collaborating to improve the appearance from GLD. More studies are needed to prove its effectiveness.
Cellasene® Gold
Cellasene® Gold is a herbal supplement developed in Italy to improve the appearance of cellulite. It contains Ginko biloba; grape seed oil; fish oil and borage oil; Centella asiatica; fucus vesiculosus (seaweed); melilotus officinalis (sweet clover); rucus acuceatus and vitamin E. Due to this association of several herbs, Cellasene® Gold acts as an antioxidant; acts on the cutaneous microcirculation, favoring lymphatic drainage and improvement of lipedema; and acts on the synthesis of collagen and on the lipolysis of adipocytes, with consequent improvement in body contour and the appearance of GLD. More studies are needed to prove its effectiveness.
Organic silicon
Silicon is a fundamental trace element for the human body and is a structural constituent of elastin, collagen, proteoglycans and endogenous glycoproteins, which form the skin’s support structures. It acts directly in the maintenance and conservation of the structure of the dermis during the skin aging process.
Studies in fibroblast culture have shown that silicon promotes the formation of bridges between hydroxylated amino acids in elastic and collagen fibers, protecting these fibers from non-enzymatic glycosylation and decreasing their rate of degradation. They act as a coenzyme in the synthesis of interstitial matrix macromolecules and reorganize the structural glycoproteins and proteoglycans of the ground substance by stimulating the grouping of polar amino acids, normalizing their hydrophilic capacity. In microcirculation, fibroblasts modify venous and lymphatic capillary permeability; in adipose tissue, they stimulate the synthesis of cyclic adenosine monophosphate (cAMP) and the hydrolysis of triglycerides, probably through a mechanism of action on the cell membrane, activating adenylcyclase. The human body, over the years, progressively loses the ability to assimilate silicon, naturally supplied by food, and therefore its oral replacement is indicated. This replacement must be done using organic silicon, as they are biologically active. Based on this fact, several companies have developed a series of organic silicon, with different activities, to act on the extracellular matrix of connective tissues, particularly on collagen fibers, and combat the signs of skin aging and skin sagging. As they act on skin sagging, they can also be used as adjuvants in improving the appearance of the GLD.
Some forms of organic silicon for oral use are:
• Exsynutriment® (Exsymol-Biotec): orthosilicic acid stabilized in marine collagen (recommended daily dose: 100-600 mg).
• Nutricolin® (Galena): choline-stabilized orthosilicic acid (recommended daily dose: 50-600 mg).
• Biosil® (Infinity Pharma): choline-stabilized orthosilicic acid (recommended daily dose: 520 mg).
• SiliciumMax® (Fagron): orthosilicic acid stabilized in maltodextrin (recommended daily dose: 50 to 600 mg).
• Monomethylsilanetriol (MMST): the MMST form of organic silicon stabilized in marine collagen, present in liquid SiliciumMax® (from Fagron) and in Neosil® tablets (MD Lab Group).
Other oral treatments
Other substances that may be indicated as coadjuvants in the oral treatment of GLD are:
• Vitis vinifera (grape seed extract): provides antioxidant properties and acts on the microvascular system.
• Fucus vesiculosus (seaweed): reduces subcutaneous adipose tissue and influences the metabolic activity of subcutaneous fat.
• Melilotus officinalis (sweet clover): promotes venous return, in creases lymphatic circulation and improves capillary resistance.
• Aesculus hippocastanum (horse chestnut): anti-inflammatory, antioxidant and anti-edema activity. Acts on peripheral, blood and lymphatic circulation, helping in vasoconstriction, favoring circulatory return and reducing fluid retention.
• Equisetum arvense (horsetail): diuretic action, stimulates skin metabolism, accelerates healing and increases skin elasticity.
• Dioscorea opposita (wild yam root): its extract regulates the release of glycerol from adipocytes that decrease the fat content in the tissue.
LYMPHATIC DRAINAGE: MANUAL OR ENDERMOLOGY
Developed by Emil and Estrid Vodder in 1936, lymphatic drainage is a technique with movements that help in the body’s lymphatic circulation, draining the accumulated fluids between the interstitial spaces and, consequently, collaborating towards tissue water balance. Manual lymphatic drainage is performed by manipulating the lymphatic vessels with hands; with this, it is possible to exert different pressures, superficial and deep, along the path of the lymphatic system, which potentiate the transport of the fluid to the lymphatic channels, reducing the intercellular edema of the adipose tissue and decreasing the metabolic ones that cause issues in the anatomical structures. Lymphatic drainage by endermology is performed with the aid of devices that combine continuous suction with constant movement of the skin and greater consistency of pressure and agility of the procedure.
Like topical therapies, lymphatic drainage (manual or by endermology) is transient and its main purpose is to reduce lymphedema associated with gynoid lipodystrophy (GLD). In this way, the reduc- tion of residues and the microcirculation of the subcutaneous tissue are promoted.
DEVICES AND TECHNOLOGIES
Intense pulsed light
The intense pulsed light (IPL) technique is a technology that emits beams of polychromatic and non-collimated light, with different wavelengths on the skin, causing thermal damage due to the energy emitted. With this, the IPL provides the subsequent repair and remodeling of collagen, stimulating its production and inducing a firmer and more homogeneous dermis, thus discreetly improving the aesthetic appearance of the GLD. However, these results are not significant or lasting.
Infrared LED
The heat on the skin generated by infrared light promotes deep dermal heating that triggers increased microcirculation, lymphatic drainage and formation of new collagen fibers. The combination of infrared LEDs with physical exercises increases the metabolic level and enhances the effects of physical activity and fat burning, which can act in the treatment of cellulite. According to some studies, infrared light, when absorbed by the body, increases the synthesis of ATP (adenosine triphosphate); this, in turn, provides energy for the cells to carry out their activities. Infrared light, in addition to helping to increase physical conditioning, by increasing ATP, has an analgesic and anti-inflammatory effect, which helps people to exercise better and for longer. It is also believed that light acts directly on fat tissues, increasing their metabolic rate and leading to greater fat burning, especially during exercise. When associated with other techniques, such as ultrasound and lymphatic drainage (manual or mechanical), LED seems to provide an even better result as an adjuvant in the treatment of GLD.
Acoustic wave therapy
Also known as extracorporeal shock wave or pulse activation therapy, it aims to improve cutaneous microcirculation, neocollagenesis and lymphatic drainage. Characterized as a safe alternative, acoustic wave therapy, already widely used in urology to fragment renal calculi, has also been used as an alternative treatment for GLD. Some studies have shown that acoustic waves in the subcutaneous tissue disrupt the sclerotic fibrous septa present in GLD; stimulate collagen remodeling in the dermis; they boost microcirculation and lymphatic flow, in addition to promoting lipolysis and reducing the thickness of subcutaneous fat. Thus, in addition to improving GLD- associated lipedema, they also improve skin elasticity and the overall appearance of cellulite/GLD.
Russian current
Russian current or Russian electrostimulation stimulates muscle tone through electrotherapy. In addition to stimulating muscle tone, with consequent improvement in skin sagging, Russian current also stimulates blood circulation in the region, with improved venous return from the lower limbs. It acts as an adjunct in the treatment of GLD.
Cryofrequency
Cryofrequency technology associates high frequency electromagnetic waves with tips that promote skin cooling. Electromagnetic waves produce heat in this organ and in the subcutaneous tissue of up to 60°C, while the cooling tips cool the upper layers of the skin to -0°C. The combination of these two temperatures generates a thermal shock in the skin tissue, with consequent tissue contraction and stimulation of collagen and elastin, as well as an improvement in skin sagging, thus acting in a supporting way in the treatment of GLD.
Microcurrents
Microcurrent procedures use electrostimulation through low-frequency, continuous or alternating currents.
The purpose of microcurrents is to accelerate cell metabolism and the elimination of liquid and waste, contributing to the improvement of lipedema associated with GLD.
VelaShape III®
VelaShape III® is a combination of bipolar radiofrequency (RF), infrared light energy, pulsed vacuum and mechanical massage (rollers). Its principle is to heat the fat cells, to lead them to apoptosis, in addition to increasing the body metabolism, which helps in the elimination of these cells naturally.
Radiofrequency and infrared light are responsible for heating the adipose cells under the skin, while the vacuum and the rollers are specially designed for mechanical massage, promoting the improvement of local lymphatic drainage. In this process, fat cells are dissolved, broken and eliminated from the body. Therefore, by reducing body fat and reducing edema, VelaShape III® acts in the treatment of GLD.
Ultrasound
The energy released by the ultrasonic waves promotes cavitation in the subcutaneous fat, that is, the formation of microbubbles inside the adipocytes, which break molecular bonds and cause chemical changes in this cell and its membrane. This leads to the mechanical disruption of its wall and liquefies its contents, facilitating the drainage of this fat. As a result, there is a reduction in the volume of adipose tissue and an improvement in body contour.
Although, in association with other techniques (such as radiofrequency), it can be used in the treatment of LGD, there is no proof of its effectiveness when used alone for that purpose. Furthermore, it is not known whether the structural changes caused by ultrasound are long-lasting.
Micro and macro focused ultrasound
Technology that emits high-intensity ultrasonic energy and causes thermal coagulation microzones between 50 and 60°C, at different depths, reaching the deep reticular dermis, the superficial musculoaponeurotic system (SMAS) and the platysma. This promotes collagen denaturation, with its immediate contraction and neocollagenesis, thus increasing the thickness of the skin and muscle fascia, improving firmness and tone, and consequent improvement in sagging. The macrofocused transducers reach the fat layer, promoting denaturation and contraction of the
subcutaneous layer, with localized fat reduction. By improving skin flaccidity and thickness, and reducing adipose tissue, its use may be indicated as an adjunct in the treatment of GLD.
CoolSculpting®
CoolSculpting® consists of a cryolipolysis technique (freezing fat cells). This is a technique that was discovered in 2007 and initially tested in pigs. In 2010, the first cryolipolysis technology approved for human use appeared, guaranteed by Harvard University under the name of CoolSculpting® and with the authorization of the Food and Drug Administration (FDA) – regulatory agency of the United States – for this purpose.
The CoolSculpting® equipment suctions the tissues and submits them to homogeneous cooling, between –7 and –10°C, for a period of one hour, the time necessary for necrosis and apoptosis of adipose cells to occur. In the weeks following the procedure, the lymphatic system eliminates these broken cells; localized fat reduction results begin to be more visible in about three weeks and reach maximum effects in approximately three months. According to a Harvard study (Rox Anderson, 2008), it is possible to eliminate between 10 and 25% of localized fat with a single CoolSculpting® session. Therefore, this technique can be indicated, associated with other methods or equipment, also as an adjunct in the treatment of GLD.

Manthus®
Manthus® is a piece of equipment that works with so-called combined therapies, consisting of a 3 MHZ frequency ultrasound, associated with an electrical stimulus generator and highly penetrating polarized currents (stereodynamic currents). Ultrasound waves have a thermal, vasodilatory effect and penetrate fat cells, promoting increased permeability of their membranes and encouraging their enzymatic activities, with a consequent decrease in the size of adipocyte cells. The stereodynamic currents stimulate the lymphatic system to expel the toxins and fats that were eliminated with the ultrasound. As a result, these currents promote a slight improvement in relation to localized fat, skin sagging and, consequently, GLD.
Radio frequency
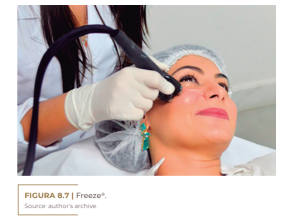
Radiofrequency (RF) energy, in the form of electromagnetic waves, has a frequency of 3 KHz to 300 Ghz, with the most used therapies ranging between 0.5 and 1.5 MHz. This energy is electrically conducted, producing an increase in tissue temperature between 38 and 40°C; through impedance, this electric current is converted into thermal energy. The energy emission mode can be monopolar, bipolar and, in the most recent devices, tripolar, hexapolar and multipolar (Freeze®).
The induction of heat in the dermal tissues (endogenous heat) triggers a series of physiological reactions, such as: local peripheral vasodilation, with consequent increase in blood flow, tissue oxygenation and cellular metabolism; it also causes immediate contraction of collagen fibers, activating fibroblasts and promoting neocollagenesis, reorganization of fibrous septa and thickening of the underlying dermal layer, with improved support, skin firmness and reduced sagging; improved lymphatic drainage, with a decrease in toxins and interstitial fluids; lysis or rupture of adipocyte membranes, with reduction in adipose tissue volume. The latter is an unproven hypothesis. RF is used in the treatment of improvement in the clinical aspect of GLD. But RF generally works best when used in combination with other techniques, such as ultrasound, infrared light, and suction lymphatic drainage. According to literature reviews, its effectiveness alone, or even in combination with other technologies, in the treatment of GLD is limited.
Freeze®
Freeze® is a multipolar radiofrequency equipment that works with eight points, creates a magnetic field between them and reaches the superficial and deep layers of the skin. This is a technology developed to reverse the effects of skin aging and indicated for the improvement and prevention of body and facial flaccidity. The magnetic pulses stimulate FGF2, the hormone responsible for the growth of blood vessels and the proliferation of fibroblasts, and, simultaneously, the high power of the radiofrequency emits electromagnetic waves, which promote an increase in the synthesis of collagen and elastin. This combination of energy will cause controlled thermal damage, stimulating self-repair mechanisms in the skin tissue, with consequent improvement in sagging associated with GLD.
Other devices
Other devices, of questionable effectiveness, that can be used to help in the treatment of GLD, are: electrolipophoresis, thermotherapy, iotonphoresis, oxygenozonotherapy and oxygenotherapy.
• Electrolipophoresis: application of several long needles in pairs, connected to a low frequency device, which create an electromagnetic field in the target tissue, triggering lipolysis and lymphatic drainage.
• Thermotherapy: use of heat for local vasodilation.
• Iontophoresis: application of galvanic current to the skin, which creates an electromagnetic field and facilitates the penetration of the active substance through the stratum corneum and promotes vasodilation.
• Oxigenozone therapy: use of oxygen and ozone gas for lipolysis. It is currently considered iatrogenic, as it promotes inflammatory and oxidative stress, with irreversible destruction of the supporting tissue.
• Oxygen therapy: excess oxygen in adipose tissue leads to lipoclasia, but, on the other hand, it can cause increased production of free radicals and biological damage due to lipoperoxidation. To avoid distant oxidative damage, it is recommended to use an ampoule of vitamin C and an ampoule of reduced glutadione (antioxidant), intravenously, one hour before oxygen therapy.
MINIMALLY INVASIVE TREATMENTS
Carboxytherapy
This technique was used for the first time in 1932, in France, in peripheral arteriopathies, but only in 1953 in the subcutaneous region. In 2004, the method was described by Brandi for aesthetic purposes after liposuction and treatment of flaccidity. The increase in the concentration of carbon dioxide (CO2) in the tissue stimulates the dissociation between oxygen and hemoglobin, causing the release of oxygen into the blood and subsequently into the tissue. This process consequently generates the expulsion of CO2 through the blood to be eliminated by the lungs (Bohr Effect). The administration of CO2 in the subcutaneous tissue induces hypercapnia and reduces the local pH, in addition to acting directly on the relaxation of the smooth muscles of the arterioles, causing significant vasodilation and improvement in microcirculation. Furthermore, the in- fusion of CO2 into the skin leads to tissue stretching and consequent sub- clinical inflammation, which promotes repair and regeneration processes, activating macrophages, fibroblasts and endothelial cells. With this, there is a remodeling of the extracellular matrix, with the formation of new collagen and elastin fibers in the treated skin and neoangiogenesis. In addition, studies show that the infiltration of CO2 gas into the sub-cutaneous adipose tissue, by improving peripheral circulation, increases tissue perfusion and the partial pressure of oxygen through reflex vasodilation, leading to an improvement in the organization of fibrous
lines and a reduction in the number and the size of the adipocytes in the treated area, improving localized fat and the orange peel aspect of cellulite (GLD), since, by reducing the accumulation of localized fat, it reduces local tissue compression, traction on fibrotic bundles and the consequent protrusion of adipocytes in the dermis, typical of GLD.
With the improvement in blood and lymphatic flows, due to the improvement in peripheral tissue perfusion promoted by CO2, there is an increase in lymphatic drainage and a decrease in lipedema associated with GLD.
Mesotherapy or intradermotherapy
Mesotherapy is a procedure developed in 1952 by Dr. Michel Pistor for the treatment of pain and vascular disorders. The term mesotherapy was first published by Pistor in a local medical journal in France in 1958, and defined by him as treatment of the mesoderm (the primary germ layer that develops into connective tissue, muscle, and the circulatory system). Mesotherapy consists of the application of intradermal injections of herbal or pharmacological actives directly in the region to be treated. Each session consists of the application of numerous superficial injections with specialized short needles and specific techniques. Injections can be intradermal or subcutaneous, although conceptually it is debatable whether the technique used in the latter would be mesotherapy, since the number of punctures and the volume injected subcutaneously do not correspond to that traditionally used in mesotherapy. Although mesotherapy is used for different purposes with different types of substances and has several reviews in the literature of its use for lipolysis and GLD, its effectiveness in treating this has not been consistently demonstrated due to substance variability and different mechanisms of action. The chapter “Injectable Treatments for Cellulite” discusses the main actives used in mesotherapy for the treatment of GLD.
Injectable collagen biostimulators
Another current option for the treatment of LGD is the use of injectable collagen biostimulators (such as poly-L-lactic acid, calcium hydroxyapatite or PMMA) in the area affected by cellulite, as these substances stimulate the production of fibroblasts and new components extracellular matrix, leading to an active renewal and remodeling of the connective tissue, with activation of collagen and elastin production, in addition to promoting angiogenesis. As a result, there is an increase in dermal thickness and density, an improvement in skin tone and firmness, in addition to improving microcirculation at a local level, improving flaccidity and the appearance of the LGD. This treatment can be performed alone or in combination with other therapies, with excellent results, especially with the Goldincision® technique.
• Poly-L-lactic acid (PLLA): microparticles of synthetic polymers of lactic acid, absorbable, semi-permanent and biodegradable, which produce an inflammatory response, through phagocytosis by tissue macrophages (encapsulation of microparticles) and subsequent fibroplasia. Half of the product is digested in six months. Its action lasts for 12 to 24 months.
• Calcium hydroxyapatite (CaHA): these are synthetic CaHA microspheres, not derived from animals and biodegradable. Its 148 The victory against cellulite chemical composition is similar to that of naturally occurring minerals in bones and teeth (synthetic analogue of the inorganic constituent of bones and teeth). The CaHA microspheres are encapsulated by a network of fibrin, fibroblasts and macrophages, with the CaHA acting as a scaffold for fibroplasia and the formation of new collagen. This process begins in up to four weeks and lasts for about twelve months. However, the clinical effects of CaHA can last from one to three years. Its elimination from the body follows the same path as metabolites from bone remains resulting from common bone fractures, which guarantees its biocompatibility and safety.
• Polymethylmethacrylate (PMMA): these are non-absorbable microspheres resulting from the polymerization of methyl methacrylate monomer. These microspheres, when injected into the human body, are encapsulated by the host’s collagen fibers and each microsphere produces an individual reaction in the body, stimulating fibroblasts to form new collagen fibers; this results in a solid, collagen-rich connective tissue, thus acting more as a tissue stimulator than as a filler per se. PMMA is the only permanent implant released by the National Health Surveillance Agency (ANVISA) and the Federal Drug Administration (FDA) – USA.
• Polycaprolactone (Ellansé®): made in the same presentation as Radiesse®, with 30% of particles with an approximate microscopy of 40 micrometers; each particle associated with a carboxymethylcellulose carrier.
SURGICAL TREATMENTS
Laser-lipolysis or laser liposuction
Liposuction is a surgery that aims to aspirate excess fat located in different regions of the body with a cannula.
Laser liposuction (or laser-lipolysis) uses a cannula, but with an optical fiber inside, which conducts a low-frequency diode laser (650 nm wavelength). This aims to break down the subcutaneous fat, facilitating
its elimination by the body itself – when in small amounts –, or facilitating its later aspiration through cannulas. When the adipocyte membrane is broken by laser energy, the trauma of fat removal later aspirated by the conventional cannula is reduced and venous coagulation is increased, with a lower incidence of hematomas and ecchymosis, which provides a faster recovery.
This laser interacts with fat cells, even those located in deeper layers, promoting the rupture of adipocytes and their liquefaction, trans- forming the triglycerides contained therein into glycerol and fatty acids, so that they are naturally removed by the lymphatic circulation. Fur- thermore, this material has an affinity for water and oxyhemoglobin; therefore, when the water is steamed, heat is generated, which stimu- lates the fibroblasts to produce collagen fibers, which brings about an organization of the reticular dermis and promotes skin retraction (skin
tightening), as well as an increase in skin thickness, with consequent treatment of sagging areas. The laser liposuction technique was approved by ANVISA, proving to be effective and safe for the reduction of GLD/cellulite and localized fat.
Superficial liposuction with autologous fat grafting
This is a technique that combines conventional superficial liposuction with a special cannula with a flattened, wedge-shaped tip, similar to a “duck bill”; was developed by Carlos Uebel, with autologous subcutaneous fat grafting. In autologous fat grafting, initially, fat is collected from the hip region or trochanteric areas and reserved for use in fat grafting. Subsequently, a superficial liposuction is performed with the wedge-shaped cannula. This cannula breaks the fibrous connective ligaments, releasing the septa that hold the skin to the fascia and subcutaneous tissue, in addition to promoting the least possible damage to the subdermal blood vessels, thus keeping the skin well vascularized. Finally, the fat collected is reinjected subcutaneously in all areas where the connective tissue septa were surgically ruptured, to fill in the region left with dead space by the procedure. At the end of the whole process, a compressive dressing is applied to the grafted area, in addition to the use of shorts with compression mesh. The bandage is maintained for three weeks and the mesh for another 30 days after the bandage is removed.
Subcision®
This is a surgical technique described in 1995 by Orentreich and Orentreich for the correction of wrinkles and depressed scars on the face. In 1997, it was described for the treatment of cellulite by Hexsel and Mazzucco.
Subcision® is indicated in cellulite for fibrous septal detachment. It is performed with the patient lying down, without association with the use of injectable products, since Subcision® itself acts as an autologous and physiological filler. This technique is described in detail in other chapters of this book.
Goldincision®
Goldincision® is a brand that involves a method developed by Brazilian surgeon Roberto Chacur that treats different aspects of cellulite, such as fibrosis, flaccidity and poor local circulation. The method combines injectable collagen biostimulators with detachment of the fibrous septa, being performed with the patient standing up, to treat, point by point, depressions in the skin, in addition to also reducing skin sagging, which is one of the causes of cellulite. This technique is also described in detail in other chapters of this book.
REFERENCES
Afonso JPJM, Tucunduva TCM, Pinheiro MVB, Bagatin E. Cellulite: a review. Surg Cosmet Dermatol. 2010;2 (3)214-19.
Allam NM, Elshorbagy RT, Eid MM, Abdelbasset WK, Elkholi SM, Eladl HM Comparison of Extracorporeal Shock
Wave Therapy versus Manual Lymphatic Drainage on Cellulite after Liposuction: A Randomized Clinical Trial.
Evid Based Complement Alternat Med. 2021 Aug 10; 2021: 9956879. doi: 10.1155/2021/9956879. Amorim CB, Ferreira TS, Pinheiro TA, Pinheiro TA, El uso de
extractos vegetales en el tratamento de la hidrolipodis- trofia ginoide (celulites). EFDeportes.com, Revista Digi- tal. Buenos Aires, Año 18, n. 188, Enero de 2014. http://www.efdeportes.com/
Arraes GCF, Funchal C. Influência dos polifenóis do chá verde na obesidade. Nutrição Brasil v.16 n.1 (2017). Doi: https://doi.org/10.33233/nb.v16i1.740 Atamoros FMP, Pérez DA, Sigall DA, Romay AAA, Gastelum
JAB, Salcedo JAP, Salgado PEE, Palacios GJG, Guerrero-Gon- zalez GA, De la Cerda RM, Olivera RMP, Soriano FR, Tinoco
ES, Hernández ECW. Evidence-based treatment for gynoid lipodystrophy: A review of the recent literature. J Cosmet Dermatol. 2018 Dec;17(6):977- 983.: 10.1111/jocd.12555. Bacci PA, Leibaschoff G. La Celulitis. Medical Books, Cáscon: 19-196, 2000. Bayrakci Tunay V, Akbayrak T, Bakar Y, Kayihan H, Ergun N.
Effects of mechanical massage, manual lymphatic drainage and connective tissue manipulation techniques on fat mass in women with cellulite. Journal of the European Academy of Dermatology and Venereology. 2010;24(2):138–
142. doi: 10.1111/j.1468-3083.2009.03355.x Celulite. Sociedade Brasileira de Dermatologia. Sbd.Org,
2017. Chacur R, Menezes HS, Chacur NMBS, Bataiolli, RO, Nardi R.
Cellulite treatment using subcision and polymethyl methacrylate filling (Goldincision®): case report. Indian Journal of Applied Research: Volume-9 | Issue-9 | September- 2019. DOI: 10.36106/ijar/6405958 Chacur, R. Ciência e Arte do Preenchimento. Editora AGE, 2018, 262 páginas.
Christ C., Brenke R., Sattler G., Gabriel G., Siems W. Boosting skin elasticity and revitalizing the dermis in cellulite and connective tissue weakness by means of extracorporeal acoustic wave therapy. Journal of Aesthetic Dermatology. 2008; 1:1–11.
Christovam, CF. Utilização tópica do silício orgânico no tratamento do envelhecimento facial. Rev Ciên Farmacêuticas Bás Aplic. 2016;29(2):109-17. Ciporkin H, Paschoal LH. Atualização terapêutica e fisiopatogênica da Lipodistrofia Ginóide (LDG) “Celulite”. Editora
Santos, São Paulo: 11-197, 1992. Efeito da Radiofrequência no envelhecimento cutâneo facial:Uma revisão. Interfisio. http://www.interfisio.com.br Friedmann DP, Vick GL, Mishra V. Cellulite: a review with a focus on subcision. Clin Cosmet Investig Dermatol. 2017: Jan;7 (10): 17-23. DOI: 10.2147/CCID.S95830. Gohil KJ, Patel JA, Gajjar AK. Pharmacological Review on Centella asiatica: A Potential Herbal Cure-all. Indian J Pharm Sci. 2010 Sep-Oct; 72(5): 546–556. doi: 10.4103/0250-474X.78519
Gomes, EA. Radiofrequência no tratamento da flacidez. 12 folhas. Hexsel D, Mazzuco R. Cellulite. In: Tosti A, Hexsel, D, editors.
Update in Cosmetic Dermatology. Mumbai: Springer-Verlag Berlin Heidelberg; 2013:21–32. Hexsel D, Weber MB, Taborda ML, Dal’Forno T, Zechmeister-Prado D. Celluqol® – instrumento de avaliação de qual- idade de vida em pacientes com celulite. Surg Cosmet Der- matol. 2011; 3 (2):96-101.
Hexsel D, Orlandi C, Zechmeister do Prado D. Botanical extracts used in the treatment of cellulite. Dermatol Surg. 2005; 2: 866- 872; discussion 872. Hexsel D, Soirefmann M. Cellulite: definition and evaluation. In: H Philippe, F Ferial, HI Maibach, A Agache, eds. Agache′s Measuring the Skin. Basel, Switzerland: Springer Interna- tional Publishing; 2017: 695-702.
Hexsel D, Soirefmann M. Cosmeceuticals for cellulite. Semin Cutan Med Surg. 2011; 30: 167-170. Hexsel DM, Dal’forno T, Hexsel CL. A validated photonumeric cellulite severity scale. J Eur Acad Dermatol Venereol. 2009 May;23(5):523-8. DOI: 10.1111/j.1468- 3083.2009.03101.x. Hexsel DM, Mazzuco R. Subcision: a treatment for cellulite. Nt J Dermatol 39:539-44, 2000. Hexsel DM, Mazzuco R. Subcision: Uma alternativa cirúrgica para lipodistrofia ginóide (“celulite”) e outras alterações do relevo corporal. An Bras Dermatol 72:27-32, 1997. Kede MPV, Sabatovich O. Dermatologia Estética. Editora Atheneu, São Paulo: 337-358, 2003.
Leonardi GR. Celulite: Prevenção e tratamento, 1a edição, Editora: Pharmabooks, São Paulo-SP-2010; Mendonça AMS, Pádua M, Ribeiro AP, Milani GB, João SMA. Confiabilidade intra e interexaminadores da fotograme-
tria na classificação do grau de lipodistrofia ginóide em mulheres assintomáticas. Fisioter. Pesqui. 2009 June: 16(2):102-106. DOI: 10.1590/S1809-29502009000200002. Orentreich DS. Orentreich N. Subcutaneous inicisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg 21:543-9, 1995. Quatresooz P, Xhauflaire-Uhoda E, Piérard Franchimont C, Piérard GE. Cellulite histopathology and related mecha- nobiology. Int J Cosmet Sci. 2006 Jun; 28(3):207- 10. DOI: 10.1111/j.1467- 2494.2006.00331.x.
Rawlings AV. Cellulite and its treatment. Int J Cosmet Sci. 2006; 28: 175-190.
Rossi ABR, Vergnanini AL. Cellulite: a review; J Eur. Acd Der- matol Vener 14: 251-262, 2000.
Rotunda AM, Avram MM, Avram AS. Cellulite: Is there a role for injectables? J Cosmet Laser Ther. 2005;7:147-54. Schonvvetter B, Soares JL, Bagatin E. Longitudinal evaluation of manual lymphatic drainage for the treatment of gynoid lipodystrophy. An. Bras. Dermatol. 2014 Oct; 89(5): 712- 718. DOI:10.1590/abd1806- 4841.20143130. Tokarska K, Tokarski S, Woźniacka A, Sysa Jędrzejowska A, Bogaczewicz J. Cellulite: a cosmetic or systemic issue? Con- temporary views on the etiopathogenesis of cellulite. Po- stepy Dermato Alergol. 2018 Oct;35(5):442-446. DOI: 10.5114/ ada.2018.77235.
Zerini I, Sisti A, Cuomo R, et al. Cellulite treatment: a com- prehensive literature review. J Cosmet Dermatol. 2015; 14: 224-240.
