ADVERSE EFFECTS AND COMPLICATIONS IN GOLDINCISION®
Content extracted from the book “Victory Against Cellulite” by Dr Roberto Chacur, Ed. AGE, 2023.
Dr. Roberto Chacur
Dr. Manuela Fassina
The few adverse events (AE) and complications result from the professional’s inexperience, use of incorrect technique or even inherent to the product, taking into account its different formulations and concentrations. Here are the most common ones:
• Bruises
• Seroma
• Cutaneous hemosiderosis
• Very superficial detachment – related to chronic stains (more than 3 months)
• We have no nodules in Goldincision®
• We have no allergic reaction to PMMA
• Possible pharmacodermia due to the use of antibiotics and anti-inflammatories
• Vitamin D intoxication in some rare cases, but when significant volumetry.
See Chapters
CHAPTER 1 - DEFINITION, HISTORY AND NOMENCLATURE
CHAPTER 2 - ONLINE QUESTIONNAIRE FOR CELLULITE CLASSIFICATION
CHAPTER 3 - LIPEDEMA: DESCRIPTION, DIAGNOSIS AND TREATMENT
CHAPTER 4 - ANATOMY OF THE GLUTE REGION APPLIED IN PRACTICE
CHAPTER 6 - INJECTABLE CELLULITE TREATMENTS
CHAPTER 7 - LASER-LIPO: INVASIVE TECHNOLOGY
CHAPTER 8 - OTHER CELLULITE TREATMENTS
CHAPTER 9 - BIOSTIMULATORY EFFECTS OF MICROSPHERE INJECTIONS INTO OVERLYING SKIN STRUCTURES
CHAPTER 10 - INFLUENCE OF HORMONES ON CELLULITE: WITH EMPHASIS ON ADIPONECTIN
CHAPTER 11 - GOLDINCISION®: A MULTIFACTORIAL APPROACH TO THE TREATMENT OF CELLULITE
CHAPTER 12 - STAINS POST-GOLDINCISION®
CHAPTER 13 - ADVERSE EFFECTS AND COMPLICATIONS IN GOLDINCISION®
With the collaboration of experienced medical professionals, Dr. Roberto Chacur brings together in this book an approach around the theme ranging from the genesis of cellulite, the proper method of evaluating and classifying, associated diseases and hormonal modulation to existing treatments, what really works and why the GOLDINCISION method is considered the gold standard.
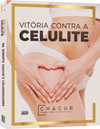
SEROMA ASPIRATION
Seroma mainly occurs when we detach an area or a larger adhesion, or when we do not act so selectively on the fibrous septum. Furthermore, this condition has a great influence on how to proceed with the patient’s follow-up, with a well-compressive dressing for at least 24 hours and modeling shorts for seven days.However, seroma happens with some frequency and decreases with the learning curve. Its management should be carried out as soon as possible and one should not wait for the revision of the procedure, which should be performed at least 40 days apart, aiming at non-encapsulation of the seroma and a lower rate of recurrence. The sooner one aspirates the content, the more minimized the relapse will be. Whether it is a seroma or a hematoma, I apply some depot corticosteroid in the region at an earlier time, with the same needle, in the same plane as the seroma capsule.
As previously mentioned, we maintain an ultrasound device in our clinics that can be very useful in some cases. In Figure 13.2, the ultrasound control of the drainage of 33 ml of hematoma is observed.
In the case of hematoma, we performed the same process, but without the need for corticoid infiltration, as it resolves with aspiration and local compression. However, in some patients, the hematoma can turn into a seroma, with aspiration no longer of bloody content, but of serous content. In this case, proceed as in the management of seroma.


Both in one and in the other, one must wait for the total resolution, in at least 45 days, without the presence of liquid, to perform a complementary procedure in the same region. We have already had patients, mainly after silicone prosthesis removal, who evolved with weekly aspiration of seroma for many months, as well as we have managed patients with Portovac drain and Penrose drain implantation, and the results were not satisfactory. Therefore, we recommend weekly aspiration with infiltration of injectable corticosteroids, always respecting an adequate dose so as not to have systemic effects due to its excessive use.
Local pressure is the most effective prevention option. A compressive bandage is used in the first 24 hours in each of the areas where the fibrous detachment was performed. An elastic compression garment should be readily available in the clinic for immediate use and should be worn for a minimum of seven days. When the bandage is removed at home, 24 hours after the procedure, an ointment should be used to treat the bruise and the garment should continue to be worn for a week. During the procedure, some blood vessels close to the septa may be sectioned, resulting in the formation of transient ecchymosis, with a risk of hematoma and seroma, which are avoided with local compression during the first 24 hours.
The patient must wear the compressive shorts provided on the day of the procedure, suspend physical activities and apply local massages for seven days, using the cosmetic products also provided by the professionals who perform the method.
NODULES
Another complication inherent to poor technique is the formation of nodules and papules, which are caused by the accumulation of product due to technical error, which includes the deposit in bolus and its superficialization.
The application with the microcannula must be carried out and kept in motion during the re-injection, as it reduces the chance of the formation of these nodules with any of the products, both with calcium hydroxyapatite with PMMA and with polylactic acid.
However, it may be a complaint for patients whose objective is volumetric gain, as the product is infiltrated in greater quantities, with twice the concentration and eventually as a liquid product, especially in the first week. With the patient’s effort, it can be partially expelled from the intramuscular tube, concentrating in a small amount in the entry hole of the microcannula.
The treatment of nodules should follow the following steps. It is important to make it clear to the patient that more than one session may be required for complete resolution.
1. Locate and delimit the nodule to be treated.
2. Asepsis of the region.
3. “Filling” the nodule with injectable anesthetic until it becomes much more palpable, and even visible, with the aid of a 30 G x 13 mm needle.
4. With the aid of a 40 G x 16 mm needle, coupled to a 10 ml syringe, apply negative pressure while fragmenting the nodule into several pieces. You will notice that the fragments will appear in the syringe, as the back and forth movement is carried out.
5. After finishing this step, apply a small dose – 0.2 ml of triocinolone deeply.
6. Instruct the patient to return after 30 days for a new evaluation.
PRODUCTS IN GELS
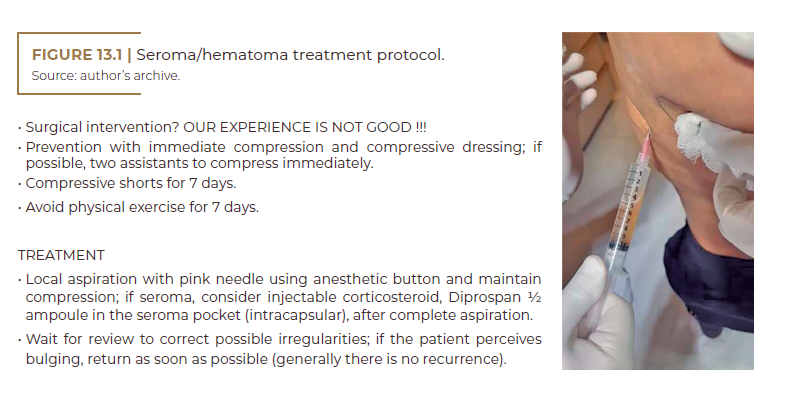
When it comes to a patient with previous procedures on the buttocks, we suggest that an MRI be performed by a qualified professional, aiming to verify the existence of gels or other products.
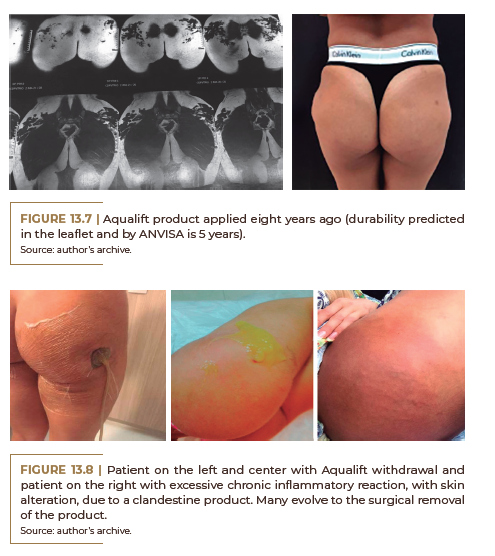
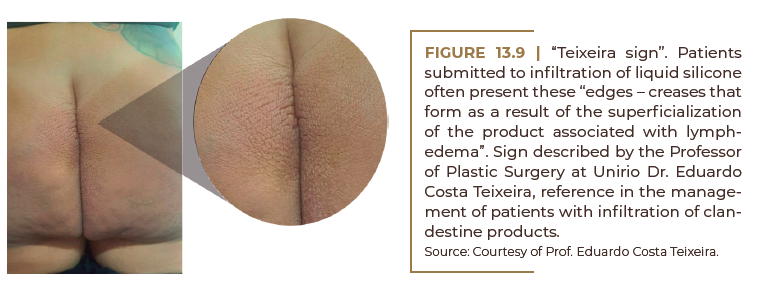
It is worth remembering that patients who previously used gels such as liquid silicone, hydrogels (Aqualift) and even hyaluronic acid should not undergo the Goldincision® technique, as we will always have an ecchymosis, which, mixed in the gels, can promote long-term changes. In addition, some gels can become infected and inflamed very easily.
![]()
The patient in Figure 13.4 had undergone an ultrasound examination performed by a radiologist with experience in liquid implants, which certified me that it would be PMMA. Outside Brazil, many clandestine products are used, but seldom is PMMA used. At the beginning of Goldincision®, see how liquid silicone flowed. In short: I have come to trust my experience and instincts more.

Aqualift (Figure 13.7) has been applied for eight years (5-year expected durability on the package insert and ANVISA). We verified that this type of product had a more fluid behavior, frequently moving to more superficial planes, with a change in relief. Many of these patients had complications (they got infected) when they decided to remove the product and when they underwent some procedure (they messed with what they shouldn’t have). Therefore, I recommend not treating patients with gel products in the buttocks.
ADDITIONAL CASE
Tissue ischemia
Often during training, doctors tend to peel off tissue very superficially at the site of cellulite. We emphasize that the detachment must be carried out as deeply and selectively as possible. We must identify and remove only the septum causing the depression and not the area as a whole.
In many cases, the identification of the area as ischemia is not early identified by the professional, who inadvertently recommends the use of cold compresses or ice, due to the presence of ecchymosis. This conduct has a negative effect on the evolution of the disease, which must be managed with local heat, a hyperbaric chamber, antibiotics while progressing to prevent a secondary infection, corticosteroids to reduce edema, antiplatelet agents, healing creams and vasodilators, with a debatable systemic vasodilator.
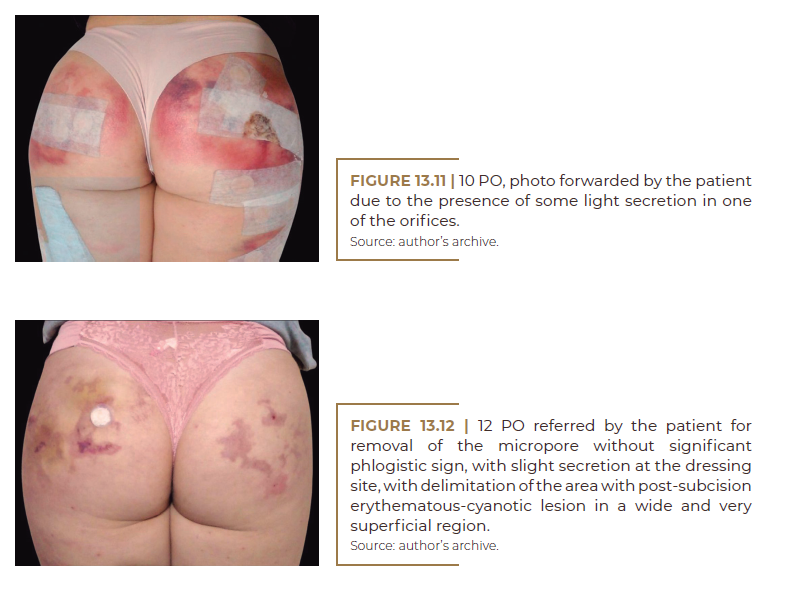
What follows is an example of tissue ischemic complication after an attempt at conventional subcision performed by a medical colleague who did not undergo Goldincision® training, who authorized the publication.
