GOLDINCISION®: A MULTIFACTORIAL APPROACH TO THE TREATMENT OF CELLULITE
Content extracted from the book “Victory Against Cellulite” by Dr Roberto Chacur, Ed. AGE, 2023.
INTRODUCTION
Goldincision® is a registered trademark that uses well-established treatment methods, such as subcutaneous detachment of cellulite fibrous septa and the use of biostimulating products (particulate products) (CHACUR et al., 2019). It is not just an association of techniques; rather, it also addresses how to carry them out: how to assess the patient; how to photograph; how to prepare the anesthetic solution; how to infiltrate (use of microcannulas); what is the infiltration plan; how to biostimulate; what products are used; how to prepare each of the products (dilution); what is the desired quantity for the treated area; what are the application protocols (how to infiltrate – using microcannulas) and what is the sequence to apply each of the techniques already used in medicine (CHACUR et al., 2019). However, after anesthesia in the regions to be treated, and after the application of the product determined by the doctor and the patient, we have the detachment of the fibrous septa, which will be performed with the patient standing up, so that the trained professional can detach each one of the irregularities accurately. In this way, it is possible to immediately visualize the correction of irregularities, which is difficult to achieve with the patient in decubitus (lying down) (CHACUR et al., 2019).
Therefore, the way to carry out each of the already recognized techniques, the evaluation and follow-up protocol, the interval between sessions and the use of techniques with compressive dressings, compressive meshes, creams to minimize and accelerate hyperchromic spots, mainly coming from the deposit of hemosiderin, are all determined by a protocol that all users of the brand must obey
See Chapters
CHAPTER 1 - DEFINITION, HISTORY AND NOMENCLATURE
CHAPTER 2 - ONLINE QUESTIONNAIRE FOR CELLULITE CLASSIFICATION
CHAPTER 3 - LIPEDEMA: DESCRIPTION, DIAGNOSIS AND TREATMENT
CHAPTER 4 - ANATOMY OF THE GLUTE REGION APPLIED IN PRACTICE
CHAPTER 6 - INJECTABLE CELLULITE TREATMENTS
CHAPTER 7 - LASER-LIPO: INVASIVE TECHNOLOGY
CHAPTER 8 - OTHER CELLULITE TREATMENTS
CHAPTER 9 - BIOSTIMULATORY EFFECTS OF MICROSPHERE INJECTIONS INTO OVERLYING SKIN STRUCTURES
CHAPTER 10 - INFLUENCE OF HORMONES ON CELLULITE: WITH EMPHASIS ON ADIPONECTIN
CHAPTER 11 - GOLDINCISION®: A MULTIFACTORIAL APPROACH TO THE TREATMENT OF CELLULITE
CHAPTER 12 - STAINS POST-GOLDINCISION®
CHAPTER 13 - ADVERSE EFFECTS AND COMPLICATIONS IN GOLDINCISION®
With the collaboration of experienced medical professionals, Dr. Roberto Chacur brings together in this book an approach around the theme ranging from the genesis of cellulite, the proper method of evaluating and classifying, associated diseases and hormonal modulation to existing treatments, what really works and why the GOLDINCISION method is considered the gold standard.
ORIGIN AND USE OF THE TERM “CELLULITE”
Cellulite is a colloquial word used to describe the deposit of fat and fibrous tissue that causes ripples in the skin. However, the suffixite, which means inflammation, is misused, as there is not always inflammation or infection of the subcutaneous tissue (MENDONÇA et al., 2009; ATAMOROS et al., 2018; Nürnberger; Müller, 1978).
The word cellulite originated in French medical literature over 150 years ago. However, the correct medical expression used for this condition is “fibrosclerotic edematous panniculopathy” or “gynoid lipodystrophy”. It is commonly known as a dermatological alteration, but there are different theories to define its concept, as explained in previous chapters (ATAMOROS et al., 2018; AFONSO et al., 2010).
TRAINING
Cellulite is much more complex than a mere accumulation of fat. The key factor is the presence of estrogen; for this reason, it occurs almost exclusively in post-pubertal women and, in fact, is present in 80 to 95% of women, in areas where fat is more predominant and where this hormone is present, such as the buttocks, thighs and hips (MENDONÇA et al., 2009; ATAMOROS et al., 2018; AFONSO et al., 2010; Emanuele; 2013).
One of the theories for the appearance of cellulite refers to the occurrence of edema in the connective tissue, which causes a large
accumulation of water and generates cellulite. Another hypothesis is the compression of the venous and lymphatic systems, which alters the microcirculation, resulting in cellulite, mainly due to the obesity factor. A third possibility is that this condition may be associated with the difference in orientation of connective tissue fibers, which are perpendicular in women and oblique in men, explaining the higher incidence of this condition in women (ATAMOROS et al., 2018; Tokarska et al., 2018; Friedmann; Vick; Mishra, 2017). The appearance of cellulite can also be influenced by collagen reduction, stress, sedentary lifestyle, obesity, heredity, hormonal contraceptives, age, sex, pregnancy, nutrition, among other factors (MENDONÇA et al., 2009; ATAMOROS et al., 2018; Nürnberger; Müller, 1978; Schonvvetter; SOARES; BAGATIN, 2014; Nürnberger, 1981).
Causes of cellulite – Theories
• Nürnberger (1981) and Müller (1978) – Different architecture in the structure of the subcutaneous tissue between men and women, with fat compartments and transverse fibers with more rectangular lobes, in addition to the fibers in the female tissue being stronger and the compressed fat resulting in the appearance of orange peel.
• Merlen (1984) and Curri (1986) – Vascular and lymphatic drainage changes, correlating with fibrosis.
• Gruber (1999) and Draelos (2005) – Correlate with the action of estrogen and the deposit of glycosaminoglycans (GAGs) by dermal fibroblasts. Adiponectin has a regulatory and insulinsensitizing metabolic function in the liver and, in muscles, it acts as an anti-inflammatory and vasculoprotective cytokine.
• Emanuele et al. (2011) – Correlated the low level of adiponectin in patients with cellulite. Adiponectin has a regulatory and insulin sensitizing metabolic function in the liver, and in muscles it acts as an anti-inflammatory and vasculoprotective cytokine.
• In September 2021, a study published in PRS (WHIPPLE et al., 2021): It was found in an ultrasound examination that in 97.6% of the cases (169 of 173 irregularities) there was the presence of a fibrous septum, and 84.4% of them had an oblique x perpendicular orientation, 90% originating from the superficial fascia, and 11 % were related to the vascular structure, in addition to being more frequent in obese or overweight people.
All were correct in their observations and all theories are correlated. The main aspect is connected to the fibrous septum. Cellulite is considered a multifactorial disease, involving circulation, poor lymphatic drainage, localized fat, flaccidity and fibrous septa. It is recognized by irregularities overlying the gluteal and thigh regions, which may be accompanied by pain, especially in the more advanced stages; and also the increase of fat nodules results in these stages. With this increase, its projection is opposed by the resistance force of the connective support trabeculae.Therefore, treatments with topical and/ or oral medications do not present very satisfactory results when used in advanced degrees of cellulite.
As it affects almost all women, it is a very common complaint in our practices, and its treatment is a real challenge, since its origin is due to the involvement of the subcutaneous connective tissue, with multifactorial causes that compromise the structure of the adipose tissue (ROSSI; VERGNANINI, 2000). The technique called Goldincision® has established itself in Brazil due to its efficacy and safety.
GOLDINCISION® METHOD
As not all the different treatments for cellulite have proven efficacy, with the Goldincision® method we seek to standardize recognized techniques in a minimally invasive way, with the patient awake, in safety and with effective results. The first step is local anesthesia, followed by biostimulation with particulate products, which help treat neocollagen and improve circulation, one of the causes of cellulite (CHACUR et al., 2019).
The standardized technique called Goldincision® has its own evaluation protocol, cellulite marking, local anesthesia and collagen biostimulation (before detachment), whose objective is to stimulate the general quality of the skin in the entire region and not punctually in cellulite. This procedure is performed with a blunt microcannula measuring 10 cm x 18 G and distributed throughout the region, always with a mobile cannula similar to that used in liposuction, so far with the patient lying down (CHACUR et al., 2019).
LOCAL ANESTHESIA
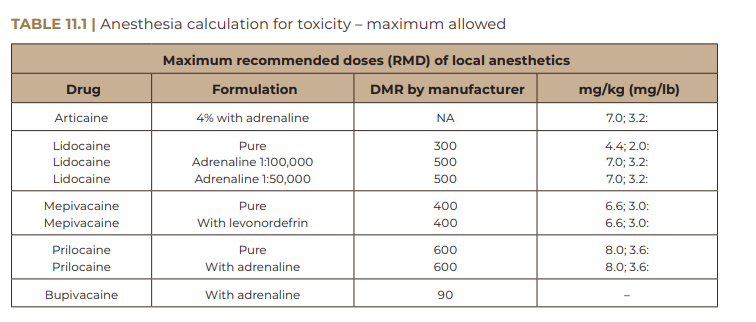
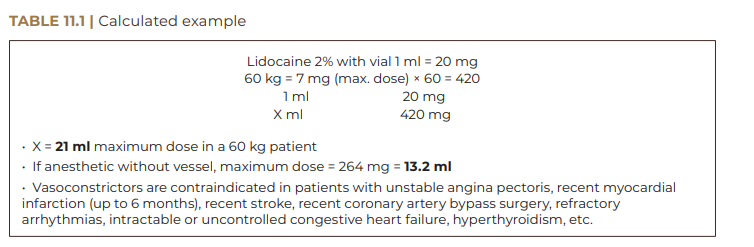
Local anesthesia is performed with 2% lidocaine with vase, diluted in a 1:1 proportion, always calculating and respecting the maximum allowed per kg, for total safety of the procedure. Anesthesia is performed with the patient in decubitus, with an orifice laterally to the right of each fibrous septum (for right-handed professionals) and preferably to the left for left-handerd professionals. The selective detachment of each septum is performed from bottom to top at each point.
Aspects observed in anesthesia:
• With the patient in the decubitus position – after marking and entry port (1 port per septum) –, anesthesia is performed only in the regions to be detached – 10 cm x 1 mm cannula.
• Lidocaine 2% with vase 1: 100,000:
° lidocaine has low toxicity compared to other anesthetics. It has a fast action, starting between 3 and 5 minutes with an average duration of 1 hour in pulp and 3 to 5 hours in soft tissues. Maximum dose: 7 mg/kg in adult patients.
• Hepatic metabolism.
• Maintain special care with the elderly, as they are more sensitive to vasoconstrictors.
• Anesthetic overdose: drowsiness, loss of consciousness and even respiratory arrest.
Table 11.1 shows the calculation performed for a patient weighing 60 kg, in which we can safely use 21 ml of 2% lidocaine anesthetic with vasopressor. In other words, we can prepare 42 ml of total solution, as described in the method, by diluting it 1:1 in saline solution. After marking in orthostatism, with the patient lying down (in decubitus), we apply the anesthetic button in each septum to be treated and the infiltration is performed with an atraumatic microcannula (blunt tip), 10 cm by 1 mm (the same one that we will use to biostimulate the region). The anesthetic should be spread only where the septal detachment will occur, always leaving a reserve (5 ml) of solution, so that we can use it at some point of greater discomfort during the detachment. Septum detachment should be performed with the patient standing, which will allow for a more accurate result, detaching as deeply and as selectively as possible only the septum, and not the region as a whole. This issue will be discussed later.
BIO-STIMULATION: LIPOSTIMULATION
In a liposuction procedure, the fat is removed symmetrically and well distributed, to avoid the risk of subdermal irregularities. As for lipostimulation, we implant particulate products with a non-volumizing objective, but as a neocollagenesis stimulator, as already discussed.
This technique can be performed with local anesthesia and microcannulas, without cuts, stitches or scars. We usually use a 10 cm long microcannula to minimize the need for more holes, generally working through a single 0.7 to 0.9 mm hole in the central gluteal region. This way, we manage to biostimulate the entire region. First, we inject the anesthesia and then the product; it is suitable to inject about 30 ml of particulate product into each buttock (never gels like Aqualift or hyaluronic acid). We know that a 20% product, either polymethylmethacrylate or calcium hydroxyapatite, or even polylactic acid (as long as it is 40 microns in diameter), is sufficient to stimulate approximately 80% of the patient’s autologous tissue (4 times more than its own volume); this is collagen-rich connective tissue (a solid tissue). Therefore, we cannot let the product accumulate on the surface, due to the risk of forming nodules, becoming palpable or even visible (Lemperle; Morhenn; Charrier, 2003; Lemperle et al., 2010). Finally, as with liposuction, the movement is the same: we can only inject the product with the cannula in motion; if we aspirate irregularly, the lipo will be irregular; if we stimulate liposuction irregularly, the product may be uneven.
BIO-STIMULATING PRODUCTS
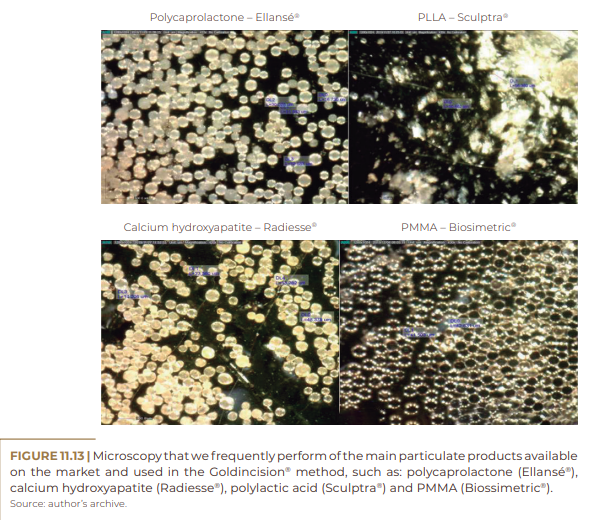
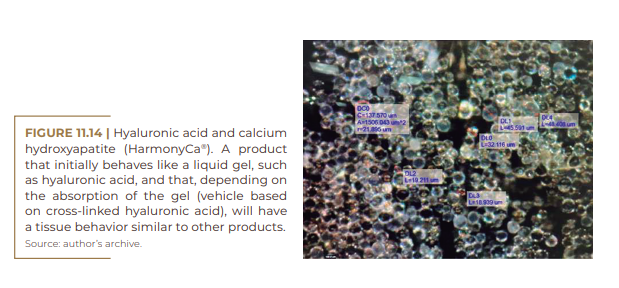
PMMA (polymethylmethacrylate – Biossimetric®), calcium hydroxyapatite (Radiesse®) and polycaprolactone (Ellansé®) are biopolymers used as fillers presented in the form of microspheres, with diameters between 40 micrometers, mixed in a suspension vehicle, such as carboxymethylcellulose or hydroxymethylcellulose. Aiming at volumetry, both manufacturers present their products in concentrations of 30%, in which we will have about 9 million particles per ml of product, which are responsible for a tissue reaction of approximately 70%, aiming to maintain the volume implanted in the treated region, where the vehicle is replaced by the patient’s own tissue, as shown in the graph in Figure 11.3.
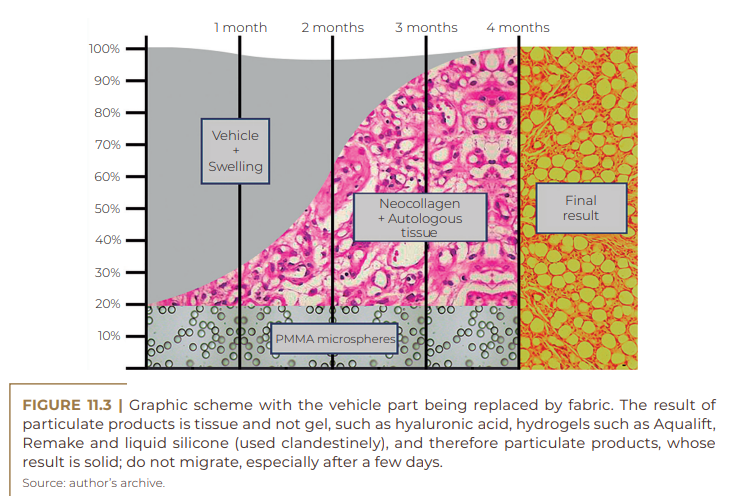
The biostimulators work with the absorption of the vehicle only and with tissue biostimulation around the particles, such as poly-L-lactic acid (Sculptra®), calcium hydroxyapatite (Radiesse®), polycaprolactone (Ellansé®) and polymethylmethacrylate (Biossimetric®). These are the main products with biostimulating action used in Brazil. With the exception of poly-L-lactic acid, which has historically been used as a biostimulator, the other products were initially used as volume boosters at a concentration of 30%. However, they can also be used as biostimulators when applied in small amounts and evenly distributed in the subdermal plane.
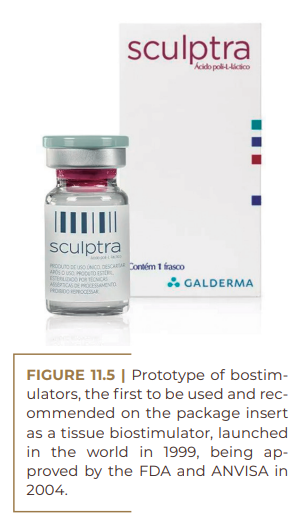
This is due to its properties of stimulating neocollagenesis through a controlled inflammatory response. Each of these products requires time for absorption and dilution, which may vary. Depending on the product, the professional needs to prepare a more diluted solution, aiming at a more uniform distribution throughout the treated area. Scuptra® was launched on the world market as a filler in 1999 and was approved by the Federal Drug Administration (FDA) – the US regulatory body – in 2004 to treat lipoaphylia in people with HIV. In addition, it lasts for approximately 1.5 years. Sculptra® is the prototype of poly-L-lactic acid. There is already another one on the market, called Rennova Elleva, which comes in powder form inside a container associated with mannitol and carboxymethylcellulose. In the past, it was recommended to dilute this substance 48 hours in advance, but recently it was seen that it was no longer necessary.
The dilution for carrying out the Goldincision® method is done only with the injection water, or, more precisely, with the creation of a 9 ml solution, which will be aspirated into 3 syringes sized 3 ml, for better precision and distribution of the product in the region to be treated. This is because we want all available anesthetic calculated according to the patient’s weight to be infiltrated at the site of the fibrous septa. Later on, we will address the general aspects of biostimulating products.

As a biostimulator, Radiesse® is diluted 1:1 in water for injection or in saline solution, transforming a concentration from 30 to 15%, for better distribution. As with the other biostimulators, we chose to concentrate as much anesthesia as possible in the areas of the fibrous septa, since the distribution of the product subdermally with a microcannula and the solution with or without anesthesia do not vary significantly, causing us to concentrate all the possible for greater patient comfort at the time of detachment of adhesions (final and main part of the procedure).
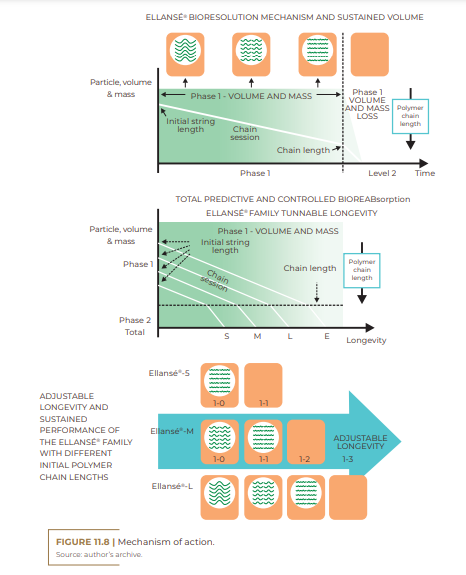
According to the manufacturer, the total bioresorption of PCL microparticles is defined by two predictable and controlled phases. The predictability of these phases defines the safety and performance of the Ellansé® Family. Unlike some other dermal fillers, which begin to bioresorb from the first day after injection, Ellansé® creates immediate and sustained performance due to the unique bioresorption pattern of PCL microspheres, where their initial mass and volume remain intact during the first phase. Eventually, after several months or years, depending on the Ellansé® longevity option chosen, the volume and mass of the fillers begin to decrease, after achieving the desired effect.
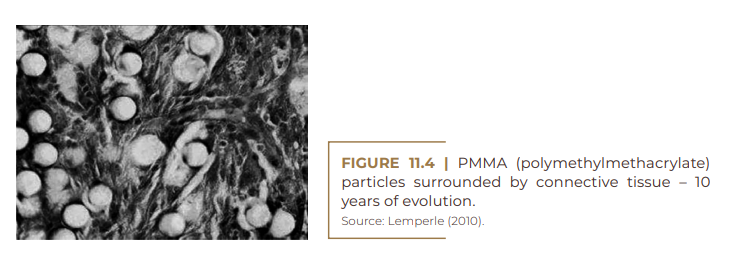
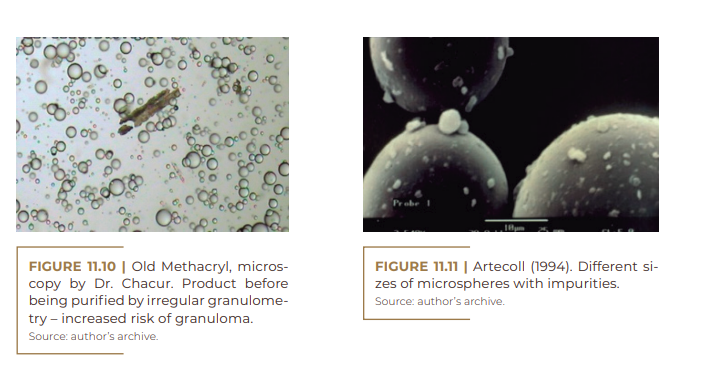
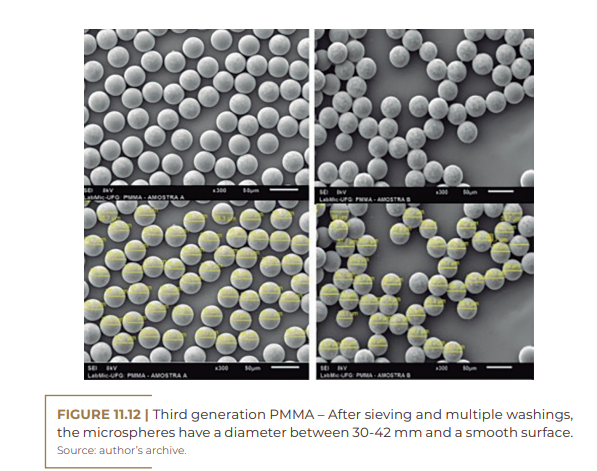
The pmma particle has undergone modifications over these 30 years. Its first generation, known as Arteplast, was made up of microspheres with an irregular surface and varying sizes, which favored the main complication, the occurrence of granulomas, with a rate of 2.5%. In 1994, laboratories began to produce smoother spheres with regular sizes, between 30 and 50 microns, which was then the second generation. With particles larger than 30 microns, it was possible to reduce the granuloma index to less than 0.01%, while the 50 microns limit prevented losses in tissue reaction and collagen stimulation.
In 2006, the filler was released by the US health agency (FDA), due to the purification of PMMA and the launch of the third generation, which brought less chances of infection, allergy and granuloma. In 2007, Anvisa prohibited the manufacture of PMMA by compounding pharmacies and started to apply a strict quality control to release the production and commercialization of the product in Brazil only by industries. Currently, PMMA is in its fourth generation, which means a product free of impurities, with regular-sized microspheres and a nanotextured surface, factors that considerably reduce the risk of granuloma, infection, allergy and rejection, and increase fixation and stimulation collagen production, according to preliminary studies released by Lemperle in 2019.
Formulated in concentrations of 5%, 10%, 15% and 30%, as well as in the dilution of Radiesse®, initially 30% diluted 1:1, Biosimetric® has already been produced specifically in this concentration to not only make life easier for the working professional, but also for the safety of being an industrialized product with this objective. In-practice mixing always poses a greater risk of contamination and a different precipitation, not allowing homogeneity in the solution, with possible precipitation of product in the vial or syringe, which may not promote equal distribution in the region to be treated. Biosimetric® with a concentration of 15% is the product of choice and approved by the Goldincision® method.
GENERAL ASPECTS ABOUT FILLERS
(Except for polylactic acid) when the objective is volume)
As with other fillers that aim for volume, we want each product to have a final volume similar to that implanted, that is, that each milliliter implanted provides me with 1 ml of final gain in volume, so that we can model our patient with a precise and with a predictable result. We do not want to implant 1 ml that increases in volume and becomes 3 ml, nor do we want to implant 3 ml that can be reduced to 1 ml, as we would not have a predictable result. Therefore, by implanting volume in the same region of identical patients, I will have a very similar volumetric aspect, whether applying hyaluronic acid or using some other hydrogels, such as Radiesse® in its original concentration of 30%; Biosimetric®, in its original concentration of 30%; or even Ellansé® in its original 30% concentration. The exception is Sculptra®, for which we have agreed on a higher dilution level and its use as a biostimulator, not for volumetric gain and change in proportion, facial or body.
Considering that these products have the same volumizing power, the final appearance (shape) of each face, for example, will be exactly the same. Thus, the ability to transform, restore volumes and work with projection, light and shadow will depend solely and exclusively on the work of the artist (professional injector). We will have each product with its peculiarities, durability, consistency, elasticity and its rheology, but the visual aspect will be the same.
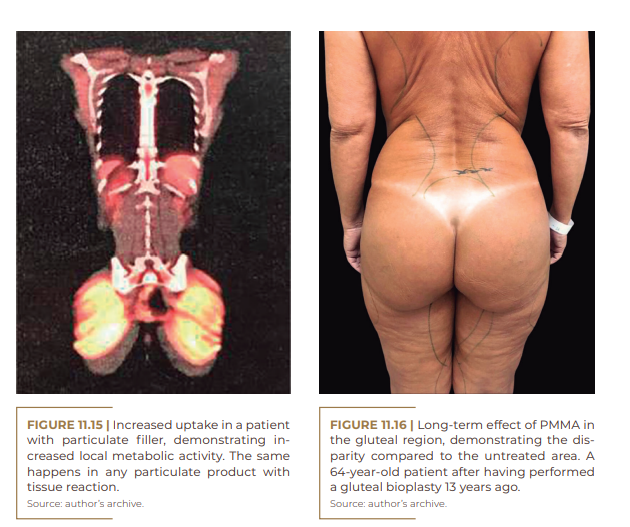
When we talk about particulate products, we are talking about living fillers, as there is a local tissue reaction, with an increase in metabolism, neovascularization and tissue stimulation with new collagen. Yes, we are acting against the very genesis of cellulite. We know that patients affected by this problem have a high amount of estrogen, with a decrease in local circulation and adiponectin, which leads to lower local metabolism. With the infiltration of particulate products, we will act on the genesis of this situation, improving the general condition of the skin and low-grade cellulite, in addition to preventing the appearance of new ones.
The pet scan is performed through the administration of a tracer, which is usually glucose marked with a radioactive substance, without damage to health and with the possibility of visualizing the regions with increased local metabolism.
In the patient above, the maintenance not only of volume, but also of collagen biostimulation over 10 years can be seen. With the exception of the lips, the toxin and the rhinoplasty, everything else was done with PMMA. The patient did not undergo lasers. An improvement in the skin is observed, even 10 years after starting treatment with PMMA alone. The patient associated total facial biostimulation at the same time (all subdermal with 10% PMMA, with emphasis on biostimulus), for skin improvement, and not a volumetric gain; at an intramuscular or just bone level, PMMA in the chin and mandible at 30%, cheekbones and dark circles at 10%. It is important to remember that when we aim to add volume, especially when it comes to long-lasting products, it should stay in the muscle, supporting it, and not on the skin, weighing it down. In this one, we put more diluted and well-distributed products, replacing the lost volume and with better consistency.
We often hear that, after the application of pmma, the patient will not be able to perform any other type of procedure in the place where he presents the product. So far, there is no device or technology that alters the implanted PMMA. We have already used it directly on the yag laser particle of the lipo-laser; short-pulse yag laser (pigment and tatoo lesion), in addition to microfocused ultrasound, with microscopy before and after the devices are installed, showing the unaltered particles.
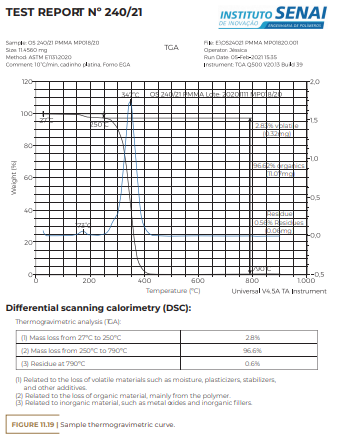
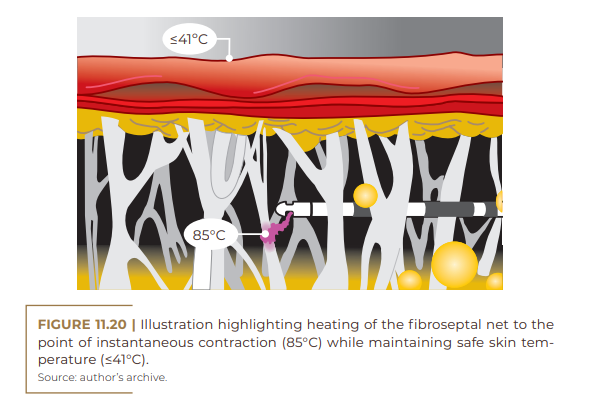
According to the report in Figure 11.19, this biopolymer is very resistant to heat. In the thermogravimetric analysis (TGA) presented in Figure 11.20, the first minimum thermal event occurred in the sample when the temperature was 135°C, and only above 250°C did relevant changes occur; today even invasive lasers, such as laser-lipo, reach temperatures of 70°C. An example is that, in the Bodytite laser, in the deepest fiber, there is between 70 and 80 °C on the skin and 85 °C with the Renuvion device (helium plasma jet technology). Thus, confirming the experiment carried out by me, forwarding the PMMA powder (particles) to colleagues who perform the lipo-laser directly on them and performing microscopy before and after, without any change in the identity of the product.
SUBCISION™
The term subcision was created by the authors David and Norman Orentreich with the contraction of the words subcutaneous and incisionless. They registered the term in the United States in 1994 and published a scientific article in Dermatol Surg in 1995 (ORENTREICH; ORENTREICH, 1995).
The authors, already at the time, cited similar techniques, including detachment, use of fillers in grooves and retraction of scars, previously published by Spangler (1957). They used the special needle used in ophthalmology “Bowman iris Needle”, which took off the scar retraction before filling it with a fibrin foam (SPANGLER, 1957). In the text, the authors also mentioned the work of Gottlieb (1977), with the development of Fibrel, a kit equipped with a needle used to remove scarring depression. They also cited the work of Koranda, who published an article in 1989 on the treatment of acne scar retraction using a “beaver blade” below the scar to detach the retraction, allowing the formation of clots to increase its elevation. Finally, David and Norman Orentreich also cited the work of Hambley and Carruthers, who, in 1992, used an 18 G needle to release adherence under a nasal skin graft before fat micrografting (Hambley; Carruthers, 1992).
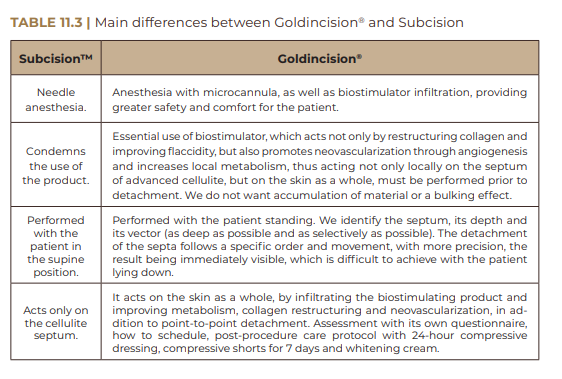
Subcision was published by David and Norman Orentreich as having one of the differentials the detachment of retractions without the need for any injectable product, as it would not be necessary, since the needle trauma itself would promote, in an autologous way (by the patient themselves), a tissue stimulus. Until then, there were several publications using detachment of scar retractions, but none without the use of fillers . Thus, this was the authors’ proposal: to carry out the previously published detachments, but without the use of fillers (NÜRNBERGER; MÜLLER, 1978). In 2000, Dr. Doris Hexsel reproduced the work that the Orentreich doctors published on scar retractions, but for cellulite retractions with the same purpose and the same name (Subcision), maintaining as a theory the non-use of fillers (HEXSEL; MAZZUCO, 2000). Therefore, if filling or biostimulating substances were used in the process, we could not call it Subcision.
Subcision, or subcision, is considered a generic name, and therefore there is no registration with the INPI as a trademark. This technique consists of detachment of fibrous septa in selected areas, with punctual results. The detachment, until then, is performed by Dr. Doris Hexsel with local anesthesia, which is infiltrated with a needle and performed with the patient lying down throughout the procedure (HEXSEL; MAZZUCO, 2000).
Goldincision® addresses not only the fibrous septa, but also the restructuring of collagen in the skin as a whole (and not in isolated spots), improving flaccidity, circulation (induction of neovascularization) and lymphatic drainage. Furthermore, the infiltration of biostimulating substances is essential (unlike in Subcision).The procedure is performed based on a holistic assessment, both static and dynamic (with the patient in movement), including the definition of the ideal product and the treatment in an orthostatic position under local anesthesia, which is fundamental, because, in this position, and only in it, can we evaluate the immediate result. We need to remove as little as possible, but enough to level out the irregularity, at the risk of causing local “bloating” in cases of excessive detachment.
HOW DID GOLDINCISION® COME ABOUT?
Goldincision® came about due to the need to treat the irregularities of patients who sought volumetric correction of the buttocks on a daily basis and were bothered by eventual irregularities. I have treated these cases in the most diverse ways, observing the advantages and disadvantages of each one of them, mainly their application forms.Initially, it would peel off with local anesthesia and the patient lying down, but the result did not seem immediate, not to mention that, often, the adhesion would form again. So, I decided to do it with the patient standing up, in order to better visualize the irregularities, even if they were previously demarcated, and I realized that in this position I was able not only to observe the irregularities, but also their evolution with the detachment, which must be the most profound and selective possible.
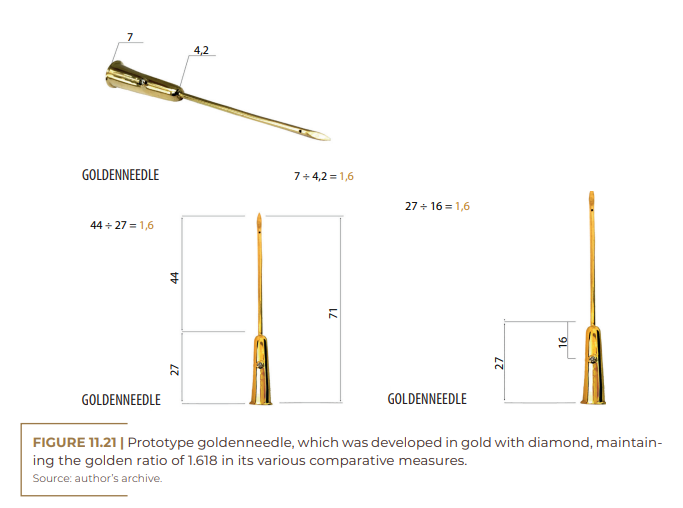
Despite that, I realized that many of them came back and that we didn’t act on the skin as a whole. So, in addition to taking it off, I filled it in, but that way I ran the risk of accumulating more product in the “loose skin” region, which could favor the appearance of nodules due to product accumulation. It was then that I realized that it was more appropriate and even safer to distribute the product without the aim of adding volume below the depression, but spreading it as a whole, thinking about improving the quality of the skin; in biostimulating; improve vascularization and local metabolism; and in the safest method, because, until then, there would be no vascular damage. Regarding the detachment devices, following the golden ratio, the LeGolden needle was developed, which is a prototype in gold with diamond, chamfered for better bilateral cutting, with an orifice that allows the introduction of local anesthetic, to reduce even the slightest discomfort of the patient. The diamond helps to signal not only the bore but also the sharp edges of the golden needle. In addition to anesthetizing with microcannulas (greater comfort), biostimulating with microcannulas and performing the treatment with the patient standing, I had to minimize risks such as hematoma, seroma and hyperpigmentation.
Management in the form of “stopping the bleeding”, with post-procedure cosmetics, compressive shorts and a compressive dressing, was described in this book. There were thousands of approaches over many years to reach the current methodology. We tried ice compression, weights, tape dressings, even gels. Today, with skilled hands, we have achieved incredible results, considered magical, recognized not only by the general population, but also by the medical community. However, it may be that, in the near future, the technique will improve even more.
Post-procedure care that prevents adverse effects and does not leave scars make Goldincision® a successful treatment with a high degree of satisfaction among patients.
GOLDINCISION® PROTOCOL
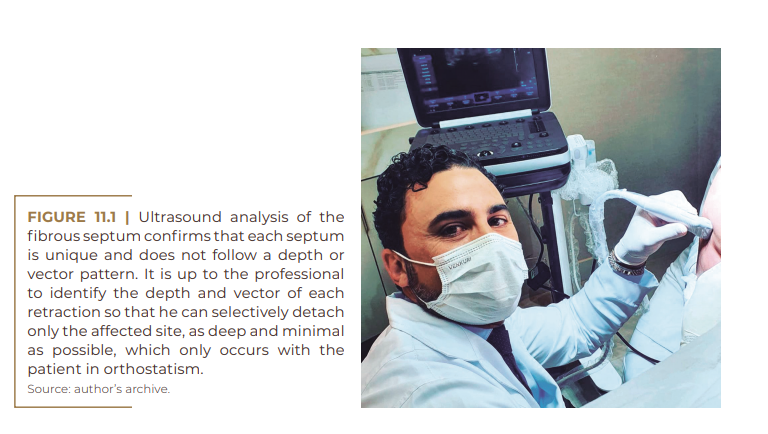
The treatment starts only after the complete analysis, informed consent, signed contract and photographic record (in some cases, video recording in motion). Ultrasonography was incorporated into the routine of our consultations, not only to better evaluate and plan our treatment, but also to help with possible complications.
After this initial procedure, with the patient in an orthostatic position, first static and then moving, all the areas that will be approached for the detachment of the fibrous septa are marked in detail, point by point. For greater comfort, local anesthesia is injected with the patient in the decubitus position, with emphasis on these areas, using a 2% lidocaine solution, in a 1:1 ratio, respecting the maximum amount calculated by the patient’s weight, generally 28 ml of solution in a 70 kg patient. This anesthetic is injected into the subcutaneous tissue of each fibrous septum with a microcannula with a blunt tip, for greater comfort and safety, as it prevents vascular trauma before injecting the biostimulator product. Biostimulators are particulate products that deliver a firm result, being calcium hydroxyapatite, polylactic acid, polycaprolactone or PMMA. Gel products such as hyaluronic acid; hydrogels, such as Aqualift, or biopolymers, such as liquid silicone, are not used. Patients with these products in their bodies should also not be included in the use of this technique.
The chosen product must be homogeneously distributed in a threedimensional way, at different depths of the subcutaneous tissue, with the aid of a microcannula (10 cm and 18 G), always in motion, similar to liposuction, for better stimulation of the neocollagen, with lower risk formation of nodules, in the entire region of the affected skin, and not just in the fibrous depression, aiming at the local biostimulation of collagen, with the aim of improving skin quality, neovascularization, increasing local metabolism and not volumizing or filling cellulite.
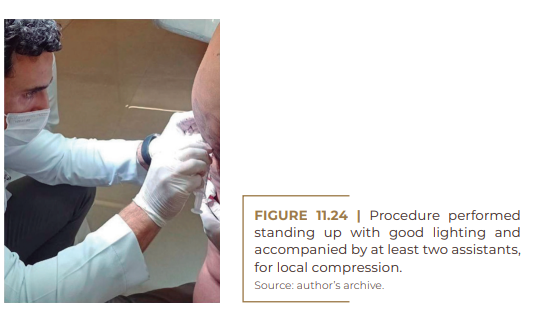
For better safety and distribution of the product, it must be placed before the fibrous detachment, to avoid accumulation in the region below the cellulite, which will be detached, with consequent nodular formation. This sequence also serves to avoid a possible embolism (common in liposculpture and very feared in fillers), since until then there will be no vascular trauma. After anesthesia in the fibrous septum and biostimulation with particulate product in the region, the most artistic part depends on the doctor’s hand and must be performed with the patient in an orthostatic position (standing), with good lighting and with the Golden needle or a single disposable needle (18 G). At the subcutaneous level, a minimal detachment is performed, which is sufficient to level the treated area point by point, as selectively as possible, always accompanied by one or two assistants, to maintain local compression.

Irregularities are loosened in a deeper subcutaneous tissue and, sometimes, using a sandwich technique, at different depths, to also avoid excessive detachment in a single plane. If this occurs, it may favor the formation of space for fluid accumulation (seroma) or even blood accumulation (bruise).
A post-treatment protocol to minimize the main adverse effects, such as hematoma and seroma, as well as a quick recovery, was necessary in the Goldincision® method. This uses a special bandage that must be kept for at least 24 hours, plus compressive shorts, which are provided on the day of the procedure, to be used for at least seven days, in addition to a cosmetic kit for better recovery and treatment of the bruise. It is important to list some mistakes that commonly happen when medical colleagues begin to perform the technique:
• Very superficial detachment – related to chronic blemishes (more than three months) and also to the chance of swelling of the skin.
• Large area detachment in the same plane – related to seroma/ hematoma.
• Detachment of some perforators and inadequate compression.
• Excessive detachment of the same lesion. Better to take off for less and complement later. In the contract, we mentioned two add-ons within six months.
• Using approved products, shorts, panties and, mainly, posttreatment kit; with that, we greatly reduced some complaints.
DISCUSSION
Cellulite, as it is commonly known, in its more advanced stages, has the clinical appearance of an orange peel. In the affected regions, the fat layer hardens, affecting the adipose tissue. Cellulite has a fibrous band in 97.6% of cases, being associated with poor circulation and metabolic failure. In adipose tissues without cellulite, there are spaces in which fat moves freely under the skin ( EMANUELE, 2011; LAUREN, 2021 ).
This clinical alteration in the skin and the risk of developing it also in the abdomen, buttocks and dorsum of the thighs cannot be related only to obesity, as there are no limitations of regions for its development in obese individuals. New improved techniques are emerging in this area, including several to improve results. In 1995, the subcision technique was described for the treatment of grades 3 and 4 cellulite, in the Nürenberger and Müller scale classification (1978).
In this technique, after photodocumentation, I mark and delimit the areas with grade 3 and 4 cellulite; then, with the patient in the decubitus position, I inject local anesthesia with an atraumatic microcannula, and then I do lipostimulation with a particulate substance. The detachment of the fibrous septum must be performed with the patient standing up, for a better identification of them, always seeking the deepest possible detachment.
CONCLUSION
Goldincision® is the registered name for a multifactorial treatment of cellulite, acting on different causes, aiming at a more effective result and at all levels of this situation. In addition to collagen remodeling, not only improving the irregular appearance and acting on sagging, there is also the detachment of fibrous septa, decompressing fat compartments, relieving local pressure and improving microcirculation, water retention and lymphatic drainage. Therefore, there is an improvement in lipedema, lymphedema and venous edema.
This technique also involves an evaluation, treatment and followup protocol, in addition to the approval of products with proven quality, with training of qualified professionals and frequent updating meetings between qualified professionals. It was possible to notice a significant improvement after performing Goldincision® in the treatment of cellulite, with a surprising degree of satisfaction from patients and the medical team, in addition to being safe and without significant adverse effects. In addition, it was also found that adiponectin (local vasodilator) is lower in patients with cellulite, reinforcing the hypothesis that the improvement in this circulation generates an improvement in appearance, which is possible with the infiltration of biostimulators.
By loosening the fibrosis, we managed to decompress the fat, reducing local pressure, improving blood flow, nutrient exchange, tissue oxygenation and lymphatic drainage, in addition to neovascularization, which the biostimulator is known to promote.All these factors help us to have a successful result and a growing demand for this treatment in our clinics.
Irregularities in the thigh regions deserve attention. In any punctual irregularity, when the patient is able to point out the cellulite, fantastic results are achieved, especially in young patients without lipedema and without sagging skin. In patients with sagging skin, mainly on the thighs, the result may not be so magical, as, somewhere, the tendency for the skin to “bend” will always exist and the eventual “banana effect” may be affected by the treatment. There is an improvement, more than with any treatment, but the result is not perfect, and occasional irregularities may be present, mainly in the buttocks and in young patients. The results in general skin quality are more related to the presence of particles than to detachment, in addition to treatments with hormonal modulations and the evaluation of other comorbidities, such as lipedema, lymphedema and venous edema.
The aesthetic appeal has been increasing a lot in recent years, especially with globalization, since beautiful images are often posted on social media with different filters, which are not consistent with reality. This takes people to an increased aesthetic perspective, where everyone looks perfect and happy, thus creating a very high standard in the world’s population. A generalized anxiety seems to take over the population.
Regardless, cellulite is a problem that affects up to 90% of the female population, causing emotional and social upheavals. Its treatment has been challenging over the centuries, as many professionals prefer not to treat or offer treatments that fall short.
Several techniques and technologies have been developed for the treatment of cellulite. However, every day I receive patients who have tried everything, with no apparent result. Multiple sophisticated devices, with laser technology, promise incredible results. They can even slightly improve the overall quality of the skin, but we don’t have a laser that can identify which fibers it needs to selectively section. For me, the need for human intervention is very clear, not only in identifying the fibrous septum, which needs detachment, but also in selective action on it, being as deep as possible, using the minimum necessary to visualize the leveling. We cannot peel more, nor do stitches unnecessarily. Devices such as Cellfina®, developed in the United States in 2015, marketed by Merz, for some time, seemed to be the solution to the problems of many professionals. However, as I already performed manual cellulite detachment a lot, I imagined that the use of the device would be restricted, with many complications and with insignificant results when compared to those that I achieved manually. Why?
The idea of this applicator was to release adhesions between the deep tissues and the skin. The device is attached to the skin through a vacuum system that pulls the cellulite region into the system.

After placing it there, small cuts 6 mm deep are automatically made, which release adhesions, removing cellulite. All this at a very high cost of equipment, as each of these applicators is for single use, that is, each complementary procedure needs to be charged as an additional procedure. Regardless of price, as already mentioned, there is no standard for cellulite. Each cellulite is unique and it is up to the professional to have the experience of being able to visualize and identify each septum, each one with its depth and each one with its vector. To do so, we first identify the cellulite, then find the septum and detach it as deeply as possible. It is very likely that it will be possible to detach it in a deeper plane, however it is only necessary to detach what is necessary, not all of the local skin, as used to be the case with the use of this applicator. One must be very selective to move the septum, and nothing more. In this way, a more evident result is achieved, without swelling, with a minimum of bruising and without that loose skin.
Furthermore, the deeper the process, the smaller the ecchymosis with residual hemosiderin, the better the recovery, the less discomfort and the faster the recovery. In other words, the artist’s manual skill will be required. Equipment promotes better skin quality, reduces local fat and improves flaccidity, but cannot selectively remove each septum in the ideal depth and quantity. Furthermore, it can be noticed, during the course of the procedure, that it must be performed under local anesthesia, so that the patient remains in orthostatism. It was the challenge of solving something that had no solution that led to the improvement of techniques and especially the way of how to conduct and in what order to carry out the treatment for cellulite. Making dreams come true, making a difference, impacting and delighting patients with the result are goals that we are achieving and offering to all those who undergo the Goldincision® technique, when performed by a qualified, trained and licensed professional.
REFERENCES
Almeida MC, Serrano CS, Roldan JR et al. Etiologia da Celulite: uma revisão. JEADV, 2013;27 :273-278.
Andre P. Evaluation of the safety of a non-animal stabilized hyaluronic acid (NASHA –Q-Medical, Sweden) in European countries: a retrospective study from 1997 to 2001. J Eur Acad Dermatol Venereol 2004;18(4):422-5.
Avram MM. Cellulite: a review of its physiology and treatment. J Cosmet Laser Ther. 2004; 6(4):181-5
Chacur R, Menezes H, Bordin N et al. Gluteal Augmentation with Polymethyl Methacrylate: A10-year Cohort Study. Plastic and Reconstructive Surgery (2019). Doi: 10.1097/ GOX.0000000000002193
Chacur R, Menezes H, Bordin N et al. Aesthetic correction of lesion by postliposuction corticoid infiltration using subcision, PMMA filling, and CO2 laser. Case Reports in Plastic Surgery and Hand Surgery (2019). Doi: 10.1080/ 23320885. 2019.1602837
Chacur R, Menezes H, Bordin N et al. Correction of Poland Syndrome (Chest Hypoplasia) Using Polymethylmethacrylate Implant. Biomedical Journal and of Scientific & Technical Research (2019). Doi: 10.26717. BJSTR.2019.14.002493
Chacur R, Menezes H, Bordin N et al. Replacement of gluteal implants by polymethyl methacrylate filler: case report. Case Reports in Plastic Surgery and Hand Surgery (2019). Doi:10.1080/23320885.2018.1549946
Christensen L, Breiting V, Janssen M et al. Adverse reactions to injectable soft tissue permanent fillers. Aesthetic Plast Surg, 2005; 29(1):34-48.
Draelos ZD, Marenus KD. Cellulite. Etiology and purported treatment. Dermatol Surg 1997;23:1177-1181.
Draelos ZD. The disease of cellulite. J Cosmet Dermatol. 2005; 4:221-211- Barbanti, V. J. Aptidão física – Um convite à saúde. São Paulo, Manole, 1990.
Elm CM, Wallander ID, Endrizzi B et al. Efficacy of a multiple diode laser system for body contouring. Lasers Surg Med, 2011; 43 . :114-121.
Ersek R. Bioplastique at 6 years: clinical outcome studies. Plast Reconst Surgery, 1997;1570-4.
Garcez CE, Implantes líquidos. In: Garcez CE, Arena-de-Souza R. Temas de Medicina Estética 2 ed Porto Alegre: Nova Prova, 2007. P.77 113.
Guirro ECO, Guirro RRJ. Fisioterapia Dermato funcional: Fundamentos, Recursos e Patologias. 3. ed. Revisada e ampliada, 2002.
Hexsel DM, Mazzuco R. Subcision: a treatment for cellulite. Int J Dermatol, 2000:39(7); 539-44.
Hexsel D, Mazzuco R. Subcision. In: Goldman M, Hexsel DM, Bacci PA, Leibashoff G. Cellulite: Pathophysiology and Treatment. Marcell-Dekker: New York, 2006.251-262.
Lotti T, Ghersetich I, Grappone C. Proteoglicanas na chamada celulite, Br J Dermatol, 1990; 29: 272-274.
McRae E, Boris J. Independent evaluation of low-level laser therapy at 635 nm for non invasive body contouring of the waist, hips, and thighs. Lasers Surg Med,2013;45:1-7.
Merlen JF, Curri SB. Anatomic-pathological causes of cellulite. J Mal Vasc 1984;9 Suppl A:53-4.
Mirrashed F, Sharp JC, Krause V et al. Tomanek Pilot study of dermal and subcutaneous fat structures by MRI in individuals who differ in gender, BMI, and cellulite grading. Skin and Research Tecnology, 2004; 10: 161-8.
Orentreich DS, Orentreich, N. Subcutaneous incisionless (Subcision®) surgery for the correction of depressed scars and wrinkles. Dermatol Surg.,1995; 21: 543-549.
Querleux B, Cornillon C, Jolivet O et al. Anatomy and physiology of subcutaneous adipose tissue by in vivo magnetic resonance imaging and spectroscopy: Relationships with sex and presence of cellulite. Skin Res Technol. 2002; 8(2):118-24.
Rao J, Glod MH, Goldman MP. A two-center, double-blinded, randomized trial testing the tolerability and efficacy of a novel therapeutic agent for cellulite reduction. J Cosmet Dermatol. 2005;4(2):93-102.
Rawlings AV. Cellulite and its treatment. Int J Cosmet Sci. 2006;28(3):175-90.
Rossi ABR, Vergnanini AL. Cellulite: a review. J Eur Acad Dermatol. Venereol 2000;14(4): 251-62.
Rossi ABR, Vergnanini AL. Celulite-uma revisão. JEAVD, 2000, 14;251-262.
Salles AG, Lotierzo PH, Gemperli R et al. Complications after polymethylmethacrylate injections: report of 32 cases. Plast Reconstr Surg, 2008;121(5):1811-20.
Sánchez CF, Tropper UP, Barceló R et al. Estudos anatomopatológico e termográfico da celulite. Rev Cosmiat Med Estet, 1994; 1 (II) :3-13.
Scherwaitz C, Braun-Falco O. So-called cellulite. J Dermatol Surg Oncol, 4: 230-234, 1978.
Smalls LK, Hicks M, Passeretti D et al. Effect of weight loss on cellulite: gynoid lypodystrophy. Plast Reconstr Surg. 2006;118(2):510-6.
Vargas AF, Amorim NG, Pintanguy I. Complicações tardias dos preenchimentos permanentes. Rev Bras Cir Plást, 2009;24(1):71-81.
