GLUTE SHAPING
Content extracted from the book “Victory Against Cellulite” by Dr Roberto Chacur, Ed. AGE, 2023.
Dr. Danuza Dias Alves
Dr. Roberto Chacur
With the aim of minimizing signs of aging and structuring the body contour, patients seek gluteal remodeling and volumetry techniques.
In ancient Greece, the body was valued for its health, athletic ability, and fertility. For the Greeks of that time, each age had its own beauty. The aesthetic, physical and intellectual aspects were part of a quest for perfection, with a beautiful body as important as a brilliant mind. In the past, beauty was considered a gift, a divine providence, a gift from heaven, and its absence was understood as an arbitrary twist of fate (SAN’T ANNA, 1995). So, the woman who was outside the aesthetic standards of the time, was condemned to accept her fate. In that period, there was no idea of individual conquest, of fighting to change one’s appearance, changing as a result of discomfort, as it exists today; we lacked intimacy with our own bodies. However, in the 21st century, there is a campaign to promote beauty, which leads to the idea that small personal efforts can lead to achieving what you want. This idea needs to be corrected because it gives the false impression of ease and absence of risks, which in practice is not true. Most of the time, what is intended is the realization of the dream of being a person with all their wishes granted and in accordance with the whims of society.
The woman, in order to be conquered, loved, strives to remain beau- tiful and attract the gaze of the man; while he needs to look attractive to please her. This helps us explain one of the great reasons why men and women seek to take care of themselves, working and modifying their bodies to attract the desire and love of others. Queiroz (1999) considers that, in Brazilian society, the most valued body part in the redefinition of symbolic topography is the butt, also euphemistically called as bumbum, an expression that is better accepted by society. Here, the butt is seen by the popular imagination as a “national preference”. In China, for instance, extremely small feet are considered beautiful and of high aesthetic value. For the feet to become disproportionately small, women submit to the harrowing effort of bandaging them so that they appear that way, a technique that generates intense pain. It is a centuries-old tradition, considered by men as erotically stimulating (FURLANI, 2003). From another perspective, according to Goldenberg (2002), there is a concern to change the look on oneself and the look of others in order to feel fulfilled. By changing the body, the individual intends to change their own life, modify their sense of identity. Cosmetic surgery is not a banal metamorphosis of a physical feature on the face or body. It operates, first of all, in the imaginary and has an impact on the individual’s relationship with the world.
See Chapters
CHAPTER 1 - DEFINITION, HISTORY AND NOMENCLATURE
CHAPTER 2 - ONLINE QUESTIONNAIRE FOR CELLULITE CLASSIFICATION
CHAPTER 3 - LIPEDEMA: DESCRIPTION, DIAGNOSIS AND TREATMENT
CHAPTER 4 - ANATOMY OF THE GLUTE REGION APPLIED IN PRACTICE
CHAPTER 6 - INJECTABLE CELLULITE TREATMENTS
CHAPTER 7 - LASER-LIPO: INVASIVE TECHNOLOGY
CHAPTER 8 - OTHER CELLULITE TREATMENTS
CHAPTER 9 - BIOSTIMULATORY EFFECTS OF MICROSPHERE INJECTIONS INTO OVERLYING SKIN STRUCTURES
CHAPTER 10 - INFLUENCE OF HORMONES ON CELLULITE: WITH EMPHASIS ON ADIPONECTIN
CHAPTER 11 - GOLDINCISION®: A MULTIFACTORIAL APPROACH TO THE TREATMENT OF CELLULITE
CHAPTER 12 - STAINS POST-GOLDINCISION®
CHAPTER 13 - ADVERSE EFFECTS AND COMPLICATIONS IN GOLDINCISION®
With the collaboration of experienced medical professionals, Dr. Roberto Chacur brings together in this book an approach around the theme ranging from the genesis of cellulite, the proper method of evaluating and classifying, associated diseases and hormonal modulation to existing treatments, what really works and why the GOLDINCISION method is considered the gold standard.
The author also points out that the body pattern based on these rules consists of highlighting certain parts of the body, developing muscles and tightening them; lifting breasts and buttocks; making the musculature strong and wide, under an ever smaller percentage of fat. The image of strength, beauty and youth becomes synonymous with health, or rather, health is subject to aesthetics, which may mean that being out of shape means to be unhealthy. Thus, the cult of the body, in the 21st century, is basically linked to two different forms of treatment: medicine and physical activity. Both treat the biological body to allow a visual implementation that pleases the body’s owner.
However, a good medical evaluation is important, as these treatments involve a series of concerns, which can lead to the most diverse courses of action. An example of this would be that they affect the psyche of the subject, who, even when changing their appearance, is not pleased with the transformation or does not satisfy their desire to model tgheir own body.
According to Freud, the narcissism of the other causes the impression of totality, of self-satisfaction. This, in turn, both fascinates us and demonstrates a person’s ability to eliminate any trace that diminishes them, that could harm them, that in some way could threaten their own
being, their self-esteem: “… it’s as if we envied them for maintaining a blissful state of mind” (FREUD, 1914).
As such, there are several options for buttock augmentation, such as silicone prosthesis, liposculpture and filling – with hyaluronic acid, hydrogels and polymethylmethacrylate.
The review entitled Gluteal Augmentation Techniques: The Comprehensive Literature Review, published in the Eathetic Surgery Journal in 2017, among the main techniques, gathered 52 studies published be- tween 1969 and 2015 (except for our own study, published in 2019 in
Plastic Reconstructive Surgery, with the use of PMMA in more than 2,700 procedures, with over 600,000 ml of product applied). The methods evaluated in this study include: 4,781 surgical cases of silicone prosthesis; 2,609 cases of liposculpture; 369 cases of gluteal flap; 69 cases of hyaluronic acid.
In the use of liposculpture, complications were at 10.5%. Although this number is lower compared to the gluteal prosthesis, the severity was greater, with cases of embolism and death being observed. Recent studies show a high rate of embolisms with the excessive filling of intramuscular fat, rates that reach one death for every three thousand patients operated in Florida in 2021.
In gluteal flaps, the rate was 22%. This percentage is apparently low when using hyaluronic acid, which, in addition to being expensive, has
the inconvenience of resulting in a temporary effect. Some of the most used techniques in the world include liposculpture,
in which the relevant fatality rate is discussed, and the gluteal prosthesis, which had its first use in 1969 in the subcutaneous plane, but with a technique that is still evolving even around 50 years later, with more promising, natural and safe results. In Brazil, the number of supporters of less invasive procedures with fillers is increasing, including PMMA, which, as published by our group in PRS, has demonstrated, in the last 16 years, a relevant case history and no case of major complications, according to Table 5.2t. All people seek to satiate their desire in some way, especially in times when the body has been given premium status. Glute filling with 30% polymethylmethacrylate (PMMA 30%) is being increasingly sought after by men and women for body remodeling, providing a natural look, in addition to a significant long-term result.
In Figure 5.3, gluteal shapes are observed, each with their peculiarities and difficulties. With the filling, unlike the silicone prosthesis, we can choose the region that we truly want to remodel, changing the shape and not just adding volume.
Among the existing fillers, we have hyaluronic acid and PMMA as current possibilities in the Brazilian market, and we already had hydrogels (Aqualift), which are no longer marketed today due to complications that have occurred, such as displacement due to greater fluidity, as time passes; lack of the promised absorption; and the high rate of infection, even within years after implanting. Our experience shows that gel products, when implanted in large volumes, show a behavior that can result in displacement over time, and the rates in this regard increase proportionally to the volume, which includes hyaluronic acid, hydrogels and even clandestinely used products, such as liquid silicone.
These materials, apparently, do not seem promising when used in large volumes, without improving the texture of the skin, such as particulate products, whose results are solid, operating as a “live filling”, in which neovascularization is maintained and created around the particles, which remain fixed in the tissue, with no migration, and nothing preventing the use of injectables or laser.
FILLING WITH PMMA
Polymethylmethacrylate is a definitive synthetic microsphere polymer inserted into a suspension vehicle, which, after being implanted, acts as a matrix (controlled inflammatory reaction), stimulating colla- gen production and muscle tissue growth. PMMA is already an implant widely used by the medical community, being the polymer of choice for bone reconstitutions and corrections, mainly due to its biocompat-
ibility characteristics, stability at the application site and low risk of complications.
The drastic evolution of product quality in recent years has directly influenced the reduction of complication rates. Currently, the PMMA available for sale in Brazil is the 4th generation, with a diameter of 40 ± 3 μm (microns). This product presents uniformity between the spheres and absence of impurities and irregularities. Therefore, the observed complications are predominantly associated with the application technique, or the lack thereof, as well as those observed with other fillers on the market. The choice of product must be cautious and in accordance with the anatomical region of application, with PMMA 30% indicated for filling glutes. This percentage is appropriate for deep implants (intramuscular), in order to avoid the occurrence of palpable nodules and possible adverse effects. Necrosis is the most feared adverse effect of the pro- cedure, but the rate attributed to this condition is 0.003%, that is, the same attributed after any filling, regardless of the product.
Polymethylmethacrylate is a synthetic product that is biocompatible with the human body, and its physical, chemical and biological characteristics, having improved over the years, have made PMMA the filler of choice for soft tissues in different concentrations (5%, 10%, 15% and 30%). Authors have already demonstrated in the literature the various uses of polymethylmethacrylate as a subcutaneous tissue biostimulator, base for bone reconstruction, intramuscular filler, among others. The increased demand for the use of PMMA for body remodeling demonstrated in this study is a consequence of the benefits it presents, as it provides a long-term result (the product is not phagocytosed by the body), without significant adverse events. It is already widely known, and the National Health Surveillance
Agency (ANVISA), through a statement, clarifies that the application of PMMA in the glutes is not contraindicated and that it is up to the doctor in charge to assess the need and feasibility of this application, which must always be cautious and with corrective purposes. Currently, in Brazil, two brands of polymethylmethacrylate are allowed by ANVISA: Biossimetric® and Linnea Safe. The use of body PMMA is for exclusive medical manipulation and its indication is only made after an evaluation consultation.
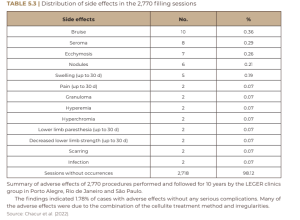
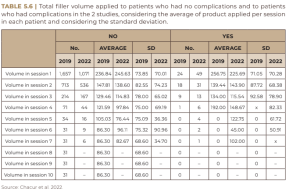
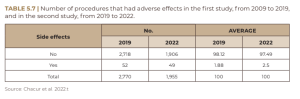
Over the 16 years of glute filling with 30% PMMA at Clínica Leger, as well as the procedures carried out for scientific publication by the team of doctors under my coordination and that of Dr. Danuza Alves,we cataloged a total of 4,725 procedures and used 922,776 ml of 30% PMMA. The average age of the patients was 39.03 years (ranging from 20 to 75 years) and the average total volume used per patient varies between 320 and 340 ml, and the complication rate varies between 1.88 and 2, 5%. Among the main complications observed, we highlight seroma, bruising, nodules and erythema.
In the past, we used a circular mold for filling. With the patient in asitting position on the stretcher and erect spine, we marked a horizontal line on the glute exactly in the region where it meets the stretcher. After this marking, with the patient in an orthostatic position, we marked the four quadrants of the glutes, above the mentioned horizontal line, with the previously mentioned template.
The orifice was performed with the patient lying in ventral decubitus, in the center of the mold, with a 40/12 needle (pink needle), after having provided the anesthetic button and, through this orifice, we performed the filling just above the marked horizontal line with a 18G/7cm cannula. Thus, we had the guarantee that we were working in a safe region and away from the emergence of most of the important vessels and nerves of the gluteus.
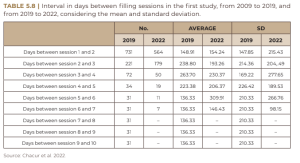
We published a multicenter article in Plastic and Reconstructive Surgery in 2019 that presents data from 1,681 patients who underwent gluteal filling at Leger clinics between 2009 and 2019.
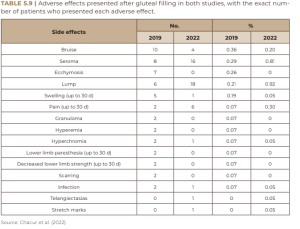
In 2022, we updated the data and published a new article on glute filling data between 2019 and 2022. Below we present the tables referring to the data found in both studies.
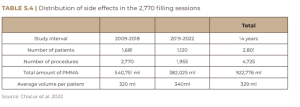
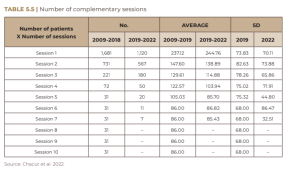
These were a total of 4725 patients in 14 years. The multicenterstudy was carried out at the Leger clinics in Rio de Janeiro, São Paulo and Porto Alegre. Almost 1 million ml of PMMA were used in the glute region alone. However, the need arose to make the shape of the glutes even more round, thus generating a demand for filling even in the lower region of the gluteus. Knowing well and reviewing the anatomy of the gluteal region, we concluded that it was possible to work in this lower region in an equally safe way, but as long as we worked in the superficial muscular plane, since the emergence of most vessels and nerves occurs in the deep muscular plane. Thus, currently, before starting the filling procedure, the patient must, first of all, sign a consent form about the situation and the respective contracts. It is essential that the patient be photographed from all angles, before and after the intervention. After taking photographs for registration, the patient is sent to the procedure room, where all the material is opened in front of the patient. Our marking is carried out with the patient in an orthostatic position. It is performed exactly in the region where there is a need for correction, which normally includes all areas of the glutes: trochanteric depression, superior pole and inferior pole. Unlike in the past, today we make multiple orifices, preferably entering perpendicularly to the areas to be corrected. It is essential that we perform correct and exhaustive asepsis with alcoholic chlorhexidine, using a procedure glove, with the patient in an orthostatic position. After asepsis, we mark all the areas to be filled, always with the patient’s collaboration, looking in the mirror and defining the areas to be corrected together with the doctor and, as previously reported, during the evaluation appointment.
After marking, with the patient lying down, we provide an anesthetic button in each of the marked orifices. By means of a 40/12 needle (pink tip needle), we carry out the orifices. A sterile field is opened with a sterile gauze on which the sterile cannula and the sterile needles that will be used are supported. All syringes that will be used during the procedure are normally opened in front of the patient, as previously mentioned, using procedure gloves; subsequently, the syringes are placed on the sterile field. Each product is opened, dividing the field into two sides, which represents the two sides of the glute, and the syringes are arranged in groups of 10 (30 ml of product), performing the exact division of the amount to be administered for each side of the glute.
After the orifices are made, using a 18G/10cm cannula, we start administering the anesthetic. For anesthesia, we prepare the solution with 2% lidocaine + 0.9% saline solution in a 1:1 dilution, obtaining a total volume of 30 ml of this solution or according to anesthetic scale with lidocaine with vasoconstrictor. We administer 15 ml of this solution on each side of the glute, distributing it over all the marked areas. After anesthesia, we start the actual filling, initially with the patient lying down and keeping the cannula always in motion, covering the marked areas. For thispurpose, the product is preferably kept in the superficial muscular plane, being able, at the time of retrograde application, to reach the very deep subcutaneous tissuein some points. We then carry out the beginning of the filling.

Preferably, only at the beginning of the procedure is the filling performed with the patient lying down. Approximately 30% of the total volume to be filled is administered in this way. After this first step, we ask the patient to stand up and, with the patient in an orthostatic position, we proceed with the filling. It is important to note that most of the filling procedure must be performed with the patient standing. The patient remains actively opining throughout the filling procedure, pointing out which area needs corrections. The patient keeps looking at themselves in the mirror all the time, deciding together with the doctor where correction is needed.
IMPORTANT CONSIDERATIONS
• The maximum safe volume for most patients is 300 ml per session; this amount must never be exceeded. We always recommend using volumes smaller than the aforementioned 300 ml per session, especially in case the professional has less experience.
• It is always better to use smaller amounts of product and a larger number of sessions.
• As a rule, the patient does not need to discontinue any of the medications of continuous use.
• Absolute contraindications for glute filling include: pregnancy, any pathology under treatment or not yet treated, according to medical evaluation.
• Relative contraindications are nephropathy, autoimmune disease, coagulopathies, extremely atopic patients, underage patients (only authorized and accompanied by parents and when indicated and absolutely necessary).
• The correction must be made with the minimum amount of product necessary.
• Pay attention to muscle contractures; when observed, the procedure should be suspended, anti-inflammatories and/or muscle relaxants should be prescribed, and the patient should be advised to return in 30 days to complete the filling.
• In the case of a patient with no skin sagging in the gluteal region, a fact observed during the physical examination in the face-to -face evaluation, preferably, the maximum volume of 120 ml of filling should never be exceeded on each side of the glute in each filling session for correction needed.
• When low muscle density is observed, making it impossible to maintain the filling procedure in the superficial muscular plane, to perform the necessary correction, one should not exceed 100 ml of filling volume on each side per session.
• Pay attention to any postural hypotension during the procedure, since the patient remains most of the time in an orthostatic position. Don’t forget that most people have pressure drops when undergoing simple lab tests.
• Check vital signs before carrying out the procedure, such as BP, especially in older patients or those with a history of SAH.
• After the filling procedure, we massage with moderate compression in the places where it was filled, after having placed a small bandage in each of the orifice areas. The bandage must be kept for 24 hours.
• The trochanteric area should always be massaged to minimize the risk of product accumulation, which can generate nodules and granulomas. The patient should be advised about edema after the procedure.
• The buttocks are usually higher (“pouty”) in the immediate post-procedure period, due to muscle contracture, which tends to increase a little more in subsequent days. Inform the patient that this aspect tends to improve in the following two weeks and that the result will be more rounded than in the immediate post-procedure period. Always prescribe the use of prophylactic antibiotics, associated with anti inflammatories, for 3 to 5 days, and a more powerful analgesic (SOS) in case of more severe pain. Muscle relaxants are a great option in case of more marked contracture and in patients with more painful symptoms.
• It is important to remember that opioid analgesics can cause dizziness and muscle relaxants can make the aptient sleepy.
• New approaches can be performed after 30 days, in case of absence of discomfort and absence of muscle contracture on physical examination. It is important to always maintain contact with the patient.
• The patient carries a labeled folder containing the batch/expiry date of the product that was used, along with the post-procedure instructions and the doctor’s contact information.
• The patient should be instructed that the volume in the immediate post-procedure usually decreases and that in most cases there is a need for a new approach to obtain the desired result. In relation to the gluteal filling areas, we highlight some particularities of clinical relevance:
• It is known that the most successful technique for performing a central or peripheral venous or arterial access is the puncture along the path of the blood vessel. We observed that the blood vessels in the gluteal region commonly run in favor of the muscle fibers, that is, parallel to them. Thus, we conclude that the safest way to perform the filling is through perpendicular openings to the area to be corrected, thus making the application safer.
• The superolateral region of the gluteal region is relatively free of nerves and vessels, making it safer.
• The region of the trochanteric area, due to the low amount of fat, is a region in which the product must be very well distributed, in order to avoid the presence of nodules and granulomas.
• The inferomedial region of the glutes is the area of emergence of nerves and vessels, which commonly exit in the deep plane; therefore, when working on this region, one should always work on the superficial muscular plane, with the smallest amount of product necessary, always keeping it well distributed.
REFERENCES
Altmeyer MD, Anderson LL, Wang AR. Silicone migration and granuloma formation. J Cosmet Dermatol. 2009;8:92– 97. [PubMed] [Google Scholar] Badin AZ, Vieira JF. Endoscopically assisted buttocks augmentation. Aesthetic Plast Surg. 2007;31:651–656. [PubMed] [Google Scholar]
Blanco Souza T, Colomé L, Bender EA, Lemperle G. Brazilian consensus recommendation on the use of polymeth- ylmetacrylate filler in facial and corporal aesthetics.
Aesth Plast Surg. 2018;42:1244–1251 [PubMed] [Google Scholar]
Cárdenas-Camarena L, Arenas-Quintana R, Robles-Cervantes JA. Buttocks fat grafting: 14 years of evolution and experience. Reconstr Surg. 2011;128:545–555. [PubMed]
[Google Scholar]
Chacur R. Ciência e Arte do Preenchimento. 2018, 1.ed Porto Alegre: AGE; 262. [Google Scholar] Chong T, Coon D, Toy J, et al. Body contouring in the male weight loss population: assessing gender as a factor in outcomes. Plast Reconstr Surg. 2012;130:325e–330e.
[PubMed] [Google Scholar] Cruse PJ, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206–210. [PubMed] [Google Scholar]
Duscher D, Kiesl D, Aitzetmüller MM, et al. Seasonal impact on surgical-site infections in body contouring surgery: a retrospective cohort study of 602 patients over a period of 6 years. Plast Reconstr Surg. 2018;142:653–660.[PubMed] [Google Scholar]
Frazer RQ, Byron RT, Osborne PB et al. PMMA: an essential material in medicine and dentistry. J Long Term Eff Med Implants. 2005;15:629–639. [PubMed] [Google Scholar]
Gonzales R. Intramuscular gluteal augmentation: the XYZ method. Clin Plastic Surg. 2018;45:217–223. [PubMed] [Google Scholar]
González-Ulloa M. Gluteoplasty: a ten-year report. Aes- thetic Plast Surg. 1991;15:85–91. [PubMed] [Google Scholar] Gruskay J, Smith J, Kepler CK et al. The seasonality of post- operative infection in spine surgery. J Neurosurg Spine.
2013;18:57–62. [PubMed] [Google Scholar] Harrison D, Selvaggi G. Gluteal augmentation surgery: indications and surgical management. J Plast Reconstr Aesthet Surg. 2007;60:922–928. [PubMed] [Google Scholar] Hilinski JM, Cohen SR. Soft tissue augmentation with Arte-
Fill. Facial Plast Surg. 2009;25:114–119. [PubMed] [Google Scholar] Jaimovich CA, Almeida MW, Aguiar LF et al. Internal suture technique for improving projection and stability in sec- ondary gluteoplasty. Aesthet Surg J. 2010;30:411–413.
[PubMed] [Google Scholar] Lee YB, Park SM, Song EJ, et al. Histology of a novel injectable filler (polymethylmethacrylate and cross-linked dextran in hydroxypropyl methylcellulose) in a rat model.J Cosmet Laser Ther. 2014;16:191–196. [PubMed] [Google Scholar]
Lemperle G, Morhenn V, Charrier U. Human histology and persistence of various injectable filler substances for softtissue augmentation. Aesthetic Plast Surg. 2003;27:354– 366; discussion 367. [PubMed] [Google Scholar]
McClelland M, Egbert B, Hanko V et al. Evaluation of artecoll polymethylmethacrylate implant for soft-tissue aug- mentation: biocompatibility and chemical characterization. Plast Reconstr Surg. 1997;100:1466–1474. [PubMed]
[Google Scholar] Mendieta CG. Gluteoplasty. Aesthet Surg J. 2003;23:441–455. [PubMed] [Google Scholar]
Oranges CM, Tremp M, di Summa PG, et al. Gluteal augmentation techniques: a comprehensive literature review. Aesthet Surg J. 2017;37:560–569. [PubMed] [Google Scholar]
Serra F, Aboudib JH, Cedrola JP, et al. Gluteoplasty: anatom- ic basis and technique. Aesthet Surg J. 2010;30:579–592.
[PubMed] [Google Scholar] Serra F, Aboudib JH, Marques RG. Intramuscular technique for gluteal augmentation: determination and quantification of muscle atrophy and implant position by computed tomographic scan. Plast Reconstr Surg. 2013;131:253e–259e. [PubMed] [Google Scholar]
Serra F, Aboudib JH, Marques RG. Reducing wound complications in gluteal augmentation surgery. Plast ReconstrSurg. 2012;130:706e–713e. [PubMed] [Google Scholar] Sozer SO, Agullo FJ, Palladino H. Autologous augmentation gluteoplasty with a dermal fat flap. Aesthet Surg J.
2008;28:70–76. [PubMed] [Google ScholarSozer SO, Agullo FJ, Palladino H. Split gluteal muscle flap for autoprosthesis buttock augmentation. Plast Reconstr Surg. 2012;129:766–776. [PubMed] [Google Scholar] Vergara R, Amezcua H. Intramuscular gluteal implants:
15 years’ experience. Aesthet Surg J. 2003;23:86–91. [PubMed] [Google Scholar]
